Edema management: Practical ways to reduce swelling fast
Swelling that won’t go down isn’t just annoying — it can signal a health problem. Edema (fluid buildup in tissues) shows up most often in ankles, feet, and hands. You don’t need fancy gear to get relief: small daily changes often make a big difference. This page collects the simplest, most useful tips so you can manage swelling and know when it’s time to see a doctor.
Quick self-care steps that actually help
Start with easy habits you can do today. Elevate swollen legs above heart level for 20–30 minutes a few times daily — that helps gravity pull fluid away. Get up and move every hour if you sit a lot; walking and ankle pumps boost circulation. Cut back on salt: processed food is the main culprit. Drink water — it sounds odd, but dehydration makes the body hold on to fluid.
Compression stockings work well for many people. Look for support labeled 15–30 mmHg for mild swelling; stronger grades need a clinician’s advice. Put stockings on in the morning before swelling starts. Wear comfortable shoes and avoid tight socks or bands that leave marks around your legs.
Simple massage toward the heart and gentle range-of-motion exercises reduce trapped fluid. Keep skin clean and moisturized to prevent cracks and infections, especially if swelling stretches the skin. Track your swelling with photos and measurements so you can see whether changes help.
When to see a doctor and medical options
See a clinician right away if swelling appears suddenly, is only on one side, is painful, or comes with shortness of breath, chest pain, fever, or lightheadedness. Those could be signs of blood clots, heart failure, kidney problems, or infection. Your doctor will ask about medicines (some blood pressure drugs, steroids, and hormones can cause edema), check your feet and legs, and may order blood tests, ultrasound, or an ECG.
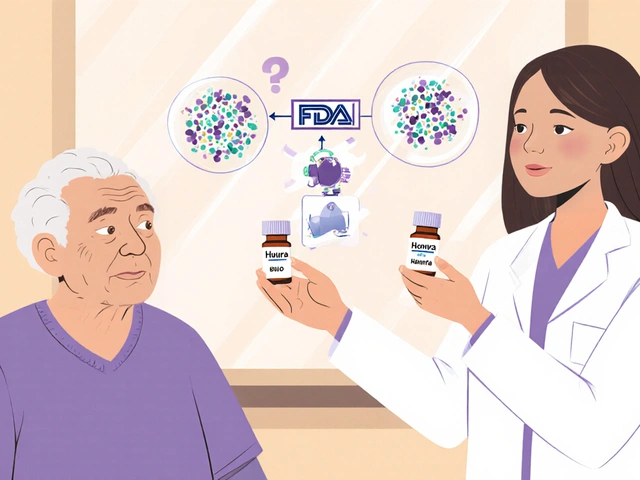
Treating the cause matters. If heart or kidney disease is behind the swelling, fixing that problem reduces edema. Doctors sometimes use diuretics (water pills) for faster relief, but dosing and follow-up matter — you need blood tests to avoid low potassium or dehydration. For chronic lymphatic swelling, manual lymphatic drainage with a trained therapist and compression bandaging can help a lot.
Practical tip: bring a list of your meds and a short diary of when swelling is worse (time of day, activity, salt intake). That makes appointments quicker and more useful. If you’re unsure, ask your provider about compression stockings, adjusting medicines, and safe exercises. Small daily habits add up — and with the right steps, most people see real improvement in a few weeks.

Lasix is popular for treating hypertension and edema, but it isn't the only option. In 2025, various alternatives like Hydrochlorothiazide provide distinctive benefits, ranging from affordability to specific health advantages. The right choice depends on individual needs and conditions, making it vital to understand each alternative's pros and cons. Here, we break down the top six Lasix substitutes for an informed decision on your health journey.