End-Stage Renal Disease: Causes, Management, and What You Need to Know
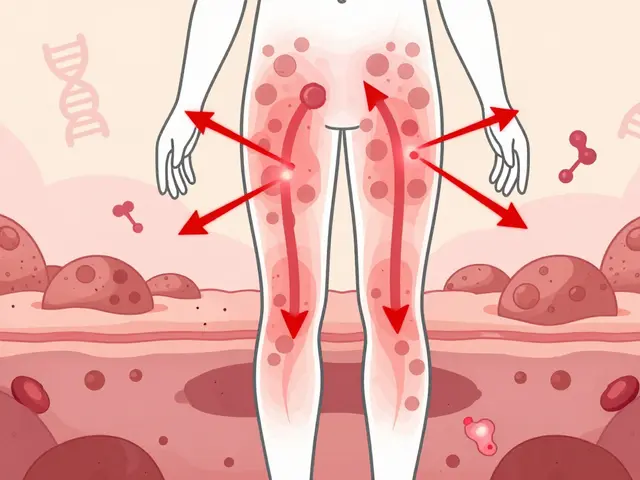
When your kidneys stop working well enough to keep you alive, you’re facing end-stage renal disease, the final stage of chronic kidney disease where the kidneys lose nearly all filtering ability. Also known as kidney failure, it’s not a sudden event—it’s the result of years of damage from diabetes, high blood pressure, or other long-term conditions. At this point, your body can’t remove waste or balance fluids on its own. Without treatment, toxins build up, swelling spreads, and your heart struggles. It’s not something you can outwait or outsmart. You need intervention.
Dialysis, a mechanical process that filters blood when kidneys can’t, is the most common lifeline. There are two types: hemodialysis, where a machine does the work outside your body, and peritoneal dialysis, where fluid in your abdomen pulls out waste. Neither is a cure, but both can let you live for years—if you stick with the schedule, manage your diet, and watch your fluids. Then there’s kidney transplant, a surgical replacement with a healthy donor kidney. It’s the closest thing to normal life after kidney failure, but it comes with lifelong anti-rejection drugs, waiting lists, and the risk of complications. What most people don’t realize is that chronic kidney disease, the slow, silent progression that leads to end-stage renal disease often starts with no symptoms at all. By the time you feel tired, swollen, or nauseous, it’s already advanced. That’s why regular blood and urine tests matter, especially if you have diabetes or high blood pressure.
Many of the posts in this collection focus on how medications, supplements, and other treatments interact with kidney function. For example, creatine supplements can raise creatinine levels and make kidney health harder to track. Statins, calcium channel blockers, and even common pain relievers need careful dosing when kidneys are failing. Some drugs are outright dangerous. Knowing how your meds are cleared—through the liver or the kidneys—can mean the difference between safety and crisis.
There’s no sugarcoating it: end-stage renal disease changes everything. But it doesn’t have to end your life. With the right treatment, support, and awareness, people live full, active lives on dialysis or after transplant. The key is understanding your options early, asking the right questions, and staying on top of your care plan. Below, you’ll find real-world guidance on managing medications, avoiding complications, and making smarter choices when your kidneys are failing.

End-stage renal disease requires life-sustaining treatment. Dialysis keeps you alive; a kidney transplant helps you live. Learn how quality of life, survival rates, and access differ between treatments-and what you can do to improve your outcomes.