Hypertension Treatment: Practical Steps to Lower Your Blood Pressure
High blood pressure doesn’t have to feel confusing. You can lower it with simple habits and the right medicines. Below I’ll walk you through what actually works so you can take action today.
Medications that work
Doctors usually pick from five main drug groups: ACE inhibitors (like lisinopril), ARBs (like losartan), thiazide diuretics (like hydrochlorothiazide), calcium channel blockers (like amlodipine), and beta-blockers (like metoprolol). Each class works differently, and sometimes two drugs from different groups are used together for better control.
Common side effects are easy to spot: cough or dizziness with ACE inhibitors, leg swelling with calcium blockers, more bathroom trips with diuretics, and fatigue with beta-blockers. Your doctor will check your kidneys and electrolytes after starting or changing treatment—this is routine and helps keep you safe.
Missing doses or stopping pills suddenly can raise your risk. If cost is a problem, ask about generics—many work the same as brand-name drugs and cost less.
Lifestyle changes that lower BP
Medication helps, but lifestyle does a lot of heavy lifting. Aim for 150 minutes of moderate exercise each week (brisk walking counts). Cut salt—try to keep sodium under about 2,000 mg daily. The DASH diet (more vegetables, fruit, whole grains, lean protein) lowers blood pressure in weeks.
Lose weight if you can: even 5–10% weight loss often drops numbers. Limit alcohol (men two drinks a day, women one) and quit smoking—both improve blood pressure and overall heart health. Treating sleep apnea, if present, often improves stubborn hypertension.
Home blood pressure checks matter. Use a validated upper-arm cuff, sit quietly for five minutes, and measure 1–2 times a day for a week to get a clear picture. Bring readings to your appointments or use a photo or app to track them. Targets vary, but many people aim for under 130/80 mmHg—your doctor will set the right goal for you.
When to act fast: if your reading is 180/120 mmHg or higher and you have chest pain, shortness of breath, vision changes, or severe headache, seek emergency care. For very high numbers without symptoms, contact your clinician that day.
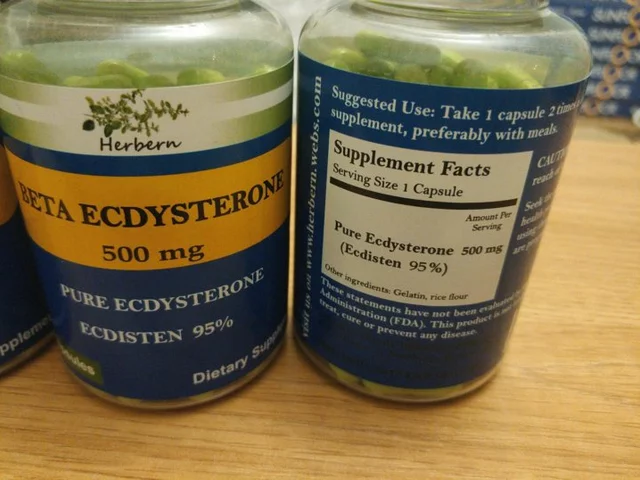
Finally, communication matters. Tell your clinician about other medicines, supplements, and side effects. If a drug causes trouble, there are usually alternatives. With the right plan—medicine, habits, and monitoring—you can lower your blood pressure and reduce long-term risks. Small steps add up quickly.

Lasix is popular for treating hypertension and edema, but it isn't the only option. In 2025, various alternatives like Hydrochlorothiazide provide distinctive benefits, ranging from affordability to specific health advantages. The right choice depends on individual needs and conditions, making it vital to understand each alternative's pros and cons. Here, we break down the top six Lasix substitutes for an informed decision on your health journey.