Polypharmacy: Risks, Risks, and How to Stay Safe with Multiple Medications
When someone takes polypharmacy, the use of five or more medications at the same time. Also known as multiple medication use, it’s not a diagnosis—it’s a situation that happens when one doctor prescribes for high blood pressure, another for arthritis, a third for sleep, and a fourth for depression. It’s common, especially in older adults, and often goes unchecked until something goes wrong. This isn’t just about taking pills—it’s about how those pills talk to each other inside your body.
Drug interactions, when one medication changes how another works are the silent danger here. Grapefruit can make blood thinners too strong. Opioids can slow your gut so much you stop having bowel movements after surgery. CYP450 enzymes in your liver—responsible for breaking down half the drugs you take—can get overwhelmed or blocked, turning safe doses into toxic ones. And it’s not just pills. Supplements, over-the-counter sleep aids, and even herbal teas can throw off the balance. You might not feel anything until you collapse from low blood pressure, get a yeast infection from a diabetes drug, or have a heart rhythm problem from an ADHD stimulant.
Medication safety, the practice of using drugs correctly to avoid harm isn’t just about following labels. It’s about asking: Why am I on all these? Can one be dropped? Is this new drug really needed, or is it just adding to the pile? Pharmacists see this every day. They’re the ones catching when a patient is on three drugs that all slow the heart, or when a kidney patient is still taking a drug that should be avoided. But they can’t fix it if they don’t know what you’re taking.
People with elderly medication use, the complex drug regimens common in older adults with multiple chronic conditions are hit hardest. Aging changes how your body absorbs, processes, and clears drugs. What was safe at 50 might be dangerous at 75. A statin that caused mild muscle pain at 60 might cause falls at 80. A sleep aid that helped you nod off might leave you confused the next morning. And when you see five different specialists, no one’s looking at the full list.
There’s no magic number that makes polypharmacy bad—five isn’t automatically wrong. But if you’re taking more than you can name, if you’re forgetting which pill is for what, or if you’ve had a side effect you can’t explain, it’s time to pause. You don’t need to stop everything. You just need someone to look at the whole picture. The posts below show real cases: how SGLT2 inhibitors cause yeast infections, how opioids delay bowel recovery, how grapefruit messes with warfarin, how statin side effects can be fixed without quitting. They’re not warnings—they’re solutions. And they’re all tied to the same problem: too many drugs, too little oversight. What you’ll find here isn’t theory. It’s what works when you’re juggling pills and trying to stay healthy.
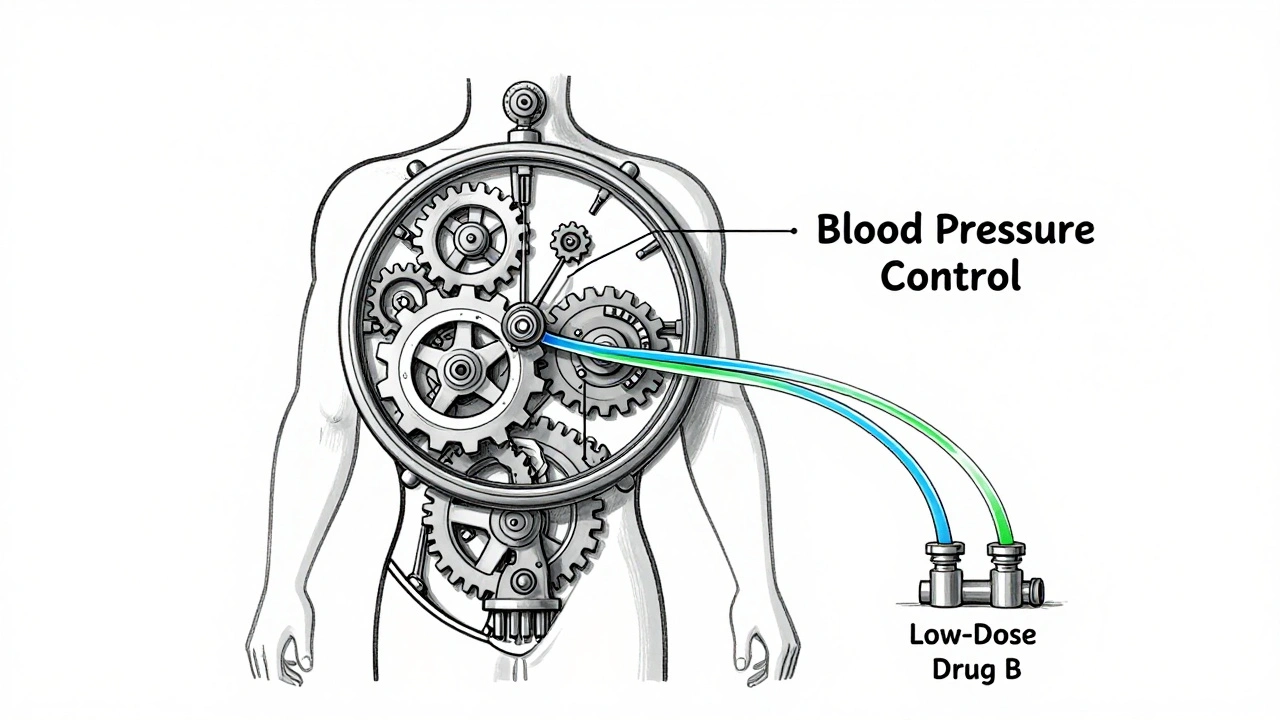
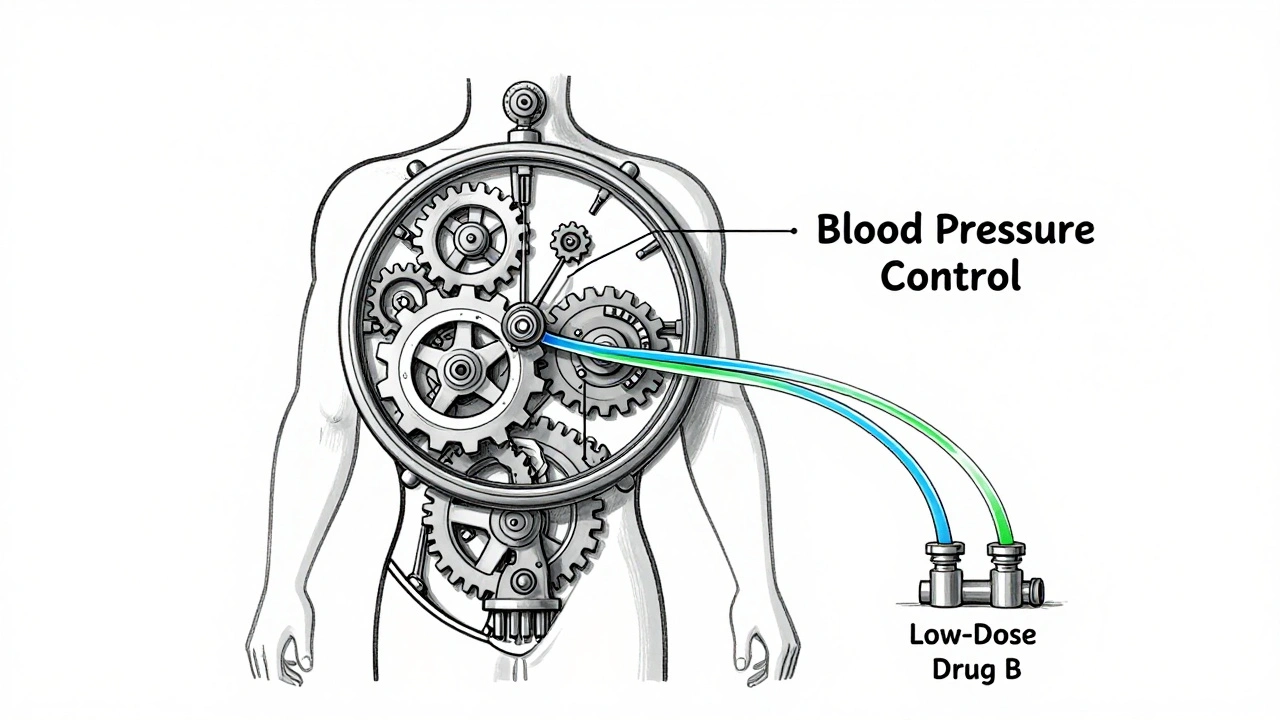
Combination therapy uses lower doses of multiple medications to improve effectiveness and reduce side effects. Proven in hypertension, diabetes, and cancer, it offers better control with fewer adverse reactions and improved patient adherence.