Drinking alcohol with diabetes isn’t off-limits-but it’s not harmless either. For many people with diabetes, a glass of wine or a beer seems like a small, normal treat. But alcohol plays tricks on your blood sugar in ways that can turn a quiet evening into a medical emergency. The biggest danger? hypoglycemia. It doesn’t always show up right away. It can sneak in hours later, even while you’re asleep. And because its symptoms-dizziness, confusion, sweating-look just like being drunk, no one might realize you’re in trouble until it’s too late.
How Alcohol Messes With Your Blood Sugar
When you drink alcohol, your liver stops doing its main job: releasing glucose into your bloodstream. That’s fine if you’re not diabetic. But if you’re on insulin or medications like sulfonylureas, your body already struggles to keep blood sugar steady. Alcohol shuts down your liver’s glucose production for up to 12 hours. That means your blood sugar can keep dropping long after you’ve finished your drink.
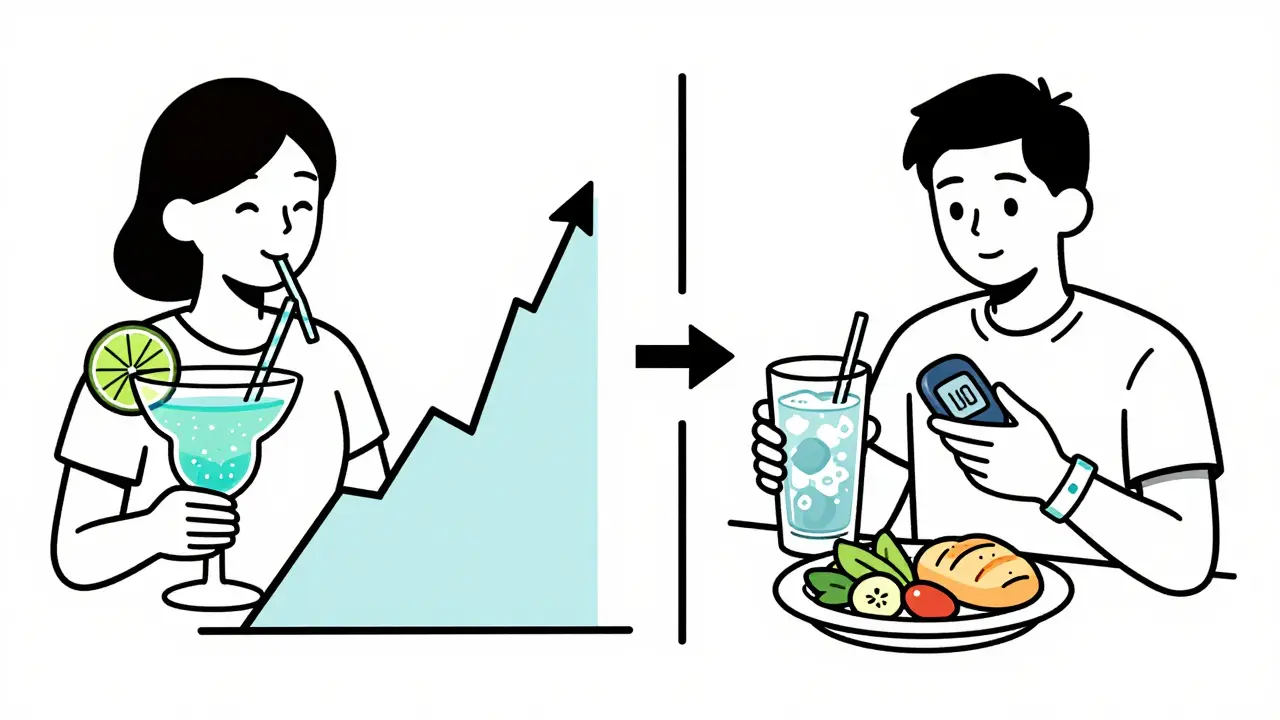
Here’s the twist: some drinks-like sweet cocktails, dessert wines, and regular soda mixers-start by spiking your blood sugar. That spike feels good. But then, as the alcohol kicks in, your liver goes quiet. Your blood sugar crashes. This two-phase effect is why people with diabetes often feel fine at first, then wake up in the middle of the night with shaking hands, a pounding heart, and confusion.
Studies show about 30% of people with type 1 diabetes who drink alcohol have had at least one severe low blood sugar episode linked to it. For those with type 2, the risk is lower but still real-especially if you’re taking insulin or pills that push your body to make more insulin.
What Counts as a Safe Drink?
Not all alcohol is created equal when you have diabetes. The key is low sugar and low carb. Here’s what’s safer:
- One 5-ounce glass of dry red or white wine (under 4g carbs)
- One 12-ounce light beer (under 5g carbs)
- One 1.5-ounce shot of vodka, gin, or whiskey with soda water or diet tonic (zero sugar)
- Hard seltzers with under 2g carbs per can
Avoid these like the plague:
- Margaritas, piña coladas, and any cocktail with juice, syrup, or regular soda (up to 25g carbs per drink)
- Sweet wines like port or sherry (they’re basically liquid candy)
- Liqueurs like Baileys or Kahlua (high sugar, high alcohol)
- ‘Diabetic’ beers or ciders-they sound safe, but they often have higher alcohol content, which increases hypoglycemia risk
Diabetes UK warns that so-called ‘low-sugar’ alcoholic drinks marketed to people with diabetes are often more dangerous because of their higher alcohol levels. More alcohol = more liver suppression = bigger drop in blood sugar.
When to Drink-And When to Absolutely Not
Don’t drink if your blood sugar is below 100 mg/dL. That’s the red line. If it’s above 300 mg/dL, wait until it’s under control. Drinking when your sugar is already high can mask how bad the problem is and make it harder to correct later.
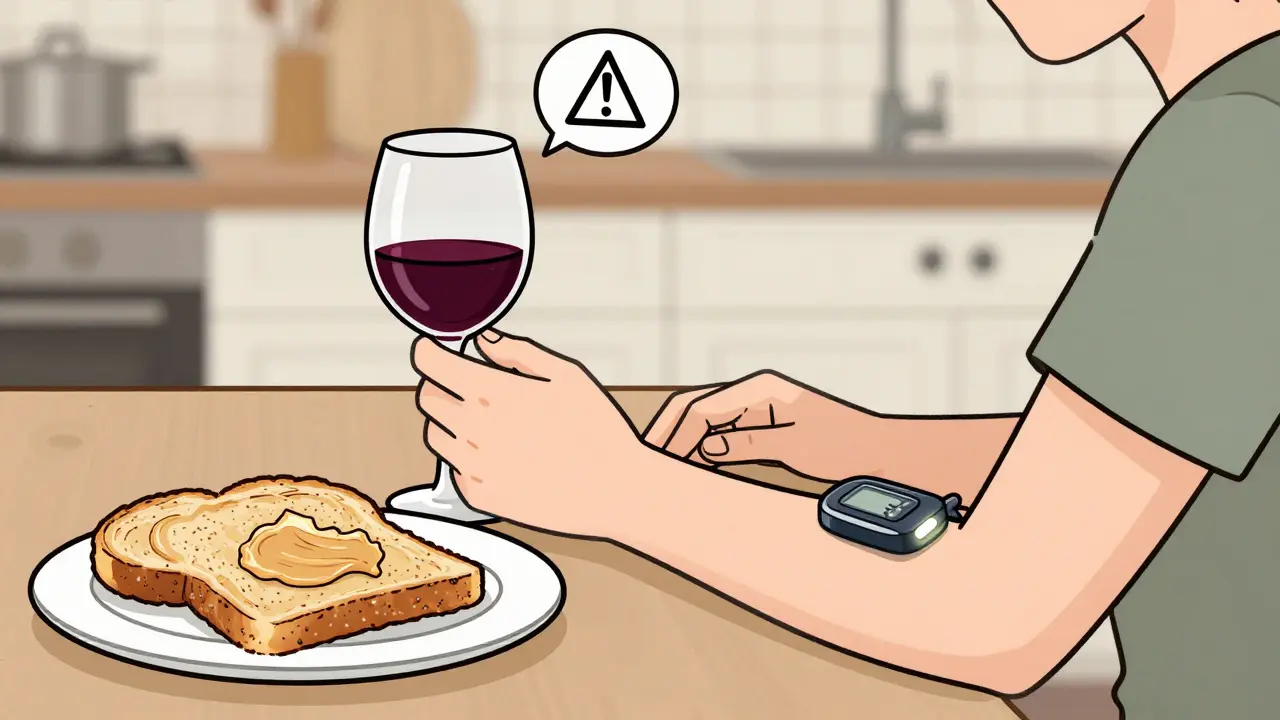
Never drink on an empty stomach. Always eat with alcohol. A meal with 15-30 grams of carbohydrates helps buffer the drop. Think: a slice of whole grain toast with peanut butter, or a small serving of rice with chicken. Don’t just snack on chips or nuts-they won’t cut it.
And never drink after exercise. Working out already lowers your blood sugar. Add alcohol? You’re stacking two hypoglycemia triggers on top of each other. Research shows this combo increases your risk of a low by 40%.

How to Drink Safely: The 4-Step Rule
If you choose to drink, follow this simple routine:
- Check your blood sugar before you start. Aim for 100-140 mg/dL. If you’re below 100, eat something first.
- Drink slowly. Sip over the course of an hour or more. Don’t chug.
- Check again every 2 hours while drinking. And check before bed-even if you feel fine. Alcohol can cause lows hours later.
- Set an alarm. If you’re at risk, wake up in the middle of the night to check your sugar. Nighttime hypos are the most dangerous.
Carry fast-acting glucose with you-glucose tablets, gel, or juice. Don’t rely on candy or regular soda. You need 15 grams of pure glucose to fix a low fast. And wear medical alert jewelry. If you pass out, someone needs to know you have diabetes.
Medications That Make Alcohol Riskier
Some diabetes drugs turn alcohol into a ticking time bomb.
- Sulfonylureas (like glipizide or glyburide): These push your pancreas to make more insulin. Add alcohol? Your insulin levels stay high while your liver stops releasing glucose. Risk of severe low blood sugar goes up by 50%.
- Insulin: The biggest risk factor. Alcohol and insulin together can cause a deep, prolonged low that’s hard to reverse.
- Metformin: Heavy drinking (more than 4 drinks in 2 hours) can trigger lactic acidosis-a rare but life-threatening buildup of acid in your blood.
If you take any of these, talk to your doctor before drinking. You might need to adjust your dose or avoid alcohol entirely.
Special Cases: Who Should Avoid Alcohol Completely?
Some people with diabetes should never drink:
- Those with diabetic neuropathy-alcohol damages nerves, and it makes numbness worse. You might not feel a low coming.
- Anyone with pancreatitis or liver disease-alcohol accelerates damage.
- Pregnant people with diabetes-no amount of alcohol is safe during pregnancy.
- People who’ve had severe hypos before-especially ones that required help from someone else.
And if you’re trying to lose weight or control your blood sugar tightly? Alcohol adds empty calories and lowers your willpower. It’s not worth the trade-off.
Technology Is Helping-But It’s Not a Fix
Some newer continuous glucose monitors (CGMs), like the Dexcom G7, now have built-in alcohol risk alerts. They can predict when your sugar might drop hours after drinking and warn you in real time. In trials, these alerts cut severe hypos by 37%.
But don’t rely on tech alone. Algorithms can’t replace your own judgment. You still need to eat, check your levels, and avoid drinking on an empty stomach. CGMs are tools-not shields.
What People With Diabetes Actually Say
On Reddit’s r/diabetes community, users share real stories. Hard seltzers get 4.5 out of 5 stars for predictability. Margaritas? 1.8 out of 5. One user wrote: ‘I thought I was just drunk after two drinks. Turns out my sugar was 42. My roommate had to give me glucose gel. I’ve never drunk since.’
Another said: ‘I drink one dry white wine with dinner every Friday. I check before bed. I eat a banana. I’m fine. It’s not about giving up-it’s about being smart.’
Seventy-three percent of negative reports mention one thing: ‘Alcohol masks the symptoms of low blood sugar.’ That’s the silent killer.
Bottom Line: It’s About Control, Not Abstinence
You don’t have to quit alcohol to manage diabetes well. But you do have to treat it like medicine-with rules, timing, and respect. The goal isn’t to scare you off. It’s to keep you safe.
Drink slowly. Eat first. Check your blood sugar before, during, and after. Know your meds. Carry glucose. Wear your medical ID. And if you’re ever unsure? Skip it. There’s no reward worth a hospital trip.
For most people with diabetes, a single drink, consumed carefully, won’t ruin your health. But one careless night? It could change everything.
Can I drink alcohol if I have type 1 diabetes?
Yes, but with strict precautions. Alcohol increases the risk of severe hypoglycemia, especially overnight. You must check your blood sugar before drinking, eat carbohydrates with it, monitor every 2 hours, and check again before bed. Always carry fast-acting glucose and wear a medical alert bracelet. Never drink after exercise or on an empty stomach.
Why does alcohol cause low blood sugar hours later?
Your liver prioritizes breaking down alcohol over releasing glucose. This suppression can last 8-12 hours. If you’re on insulin or medications that increase insulin, your body keeps using up glucose without replacing it. That’s why lows often happen while you’re sleeping-your liver isn’t doing its job, and your meds are still working.
Is red wine good for type 2 diabetes?
Some studies show moderate red wine (one glass a day) may slightly improve insulin sensitivity. But the American Diabetes Association doesn’t recommend starting to drink for health benefits. The risks of hypoglycemia, weight gain, and poor judgment outweigh any small benefit. If you already drink, stick to dry red wine-but don’t start just because you heard it’s healthy.
What’s the safest alcoholic drink for someone with diabetes?
The safest options are dry wines (red or white), light beers, hard seltzers with under 2g carbs, or distilled spirits (vodka, gin, whiskey) mixed with zero-calorie soda water or diet tonic. Avoid sugary mixers, sweet wines, and cocktails. Always check the carb label-even drinks labeled ‘light’ can have hidden sugars.
Can alcohol make diabetes worse over time?
Yes, if used regularly or irresponsibly. Heavy drinking can damage your liver, worsen nerve damage (neuropathy), increase blood pressure, and make it harder to control your weight. It can also interfere with your motivation to eat well or take medications. For people with type 2 diabetes, long-term heavy use raises the risk of pancreatitis and liver disease.
Should I avoid alcohol if I’m on metformin?
You can drink in moderation, but avoid heavy drinking. More than 4 drinks in 2 hours increases your risk of lactic acidosis-a rare but dangerous buildup of acid in your blood. Stick to one or two drinks occasionally, never on an empty stomach, and never after exercise. Always talk to your doctor about your personal risk.
Why do some people with diabetes get hypos after drinking even if they checked their sugar before?
Because alcohol’s effect is delayed. Your liver shuts down glucose production hours after you finish drinking. A normal pre-drink check might show 120 mg/dL, but if you didn’t eat enough carbs, or if you’re on insulin, your sugar can drop to 50 mg/dL by 2 a.m. That’s why checking before bed is non-negotiable.
Is it safe to drink alcohol while using an insulin pump?
It’s possible, but risky. Alcohol can cause unpredictable blood sugar swings, and your pump can’t always adjust fast enough. Many people lower their basal rate by 20-30% for 8-12 hours after drinking, but only under medical guidance. Never turn off your pump. Always carry glucose and check your levels manually, even if your pump looks fine.




January 10, 2026 AT 12:24
Alcohol and diabetes? I’ve been there. One glass of wine, thought I was fine, woke up at 3 a.m. shaking like I had the chills. My CGM screamed ‘LOW’-42 mg/dL. I didn’t even know I was that close to passing out. Now I eat a banana, check before bed, and set two alarms. It’s not about quitting. It’s about not dying stupidly.