Choosing the right insulin regimen isn’t just about numbers on a glucose meter-it’s about how well it fits your life, your schedule, and your body’s response. For people with diabetes, especially type 2 but also type 1, two main insulin strategies dominate: basal-bolus and premixed insulin. Both lower blood sugar. But they do it in very different ways, and those differences shape everything from how often you get low blood sugar to whether you can skip lunch without panic.
How Each Regimen Works
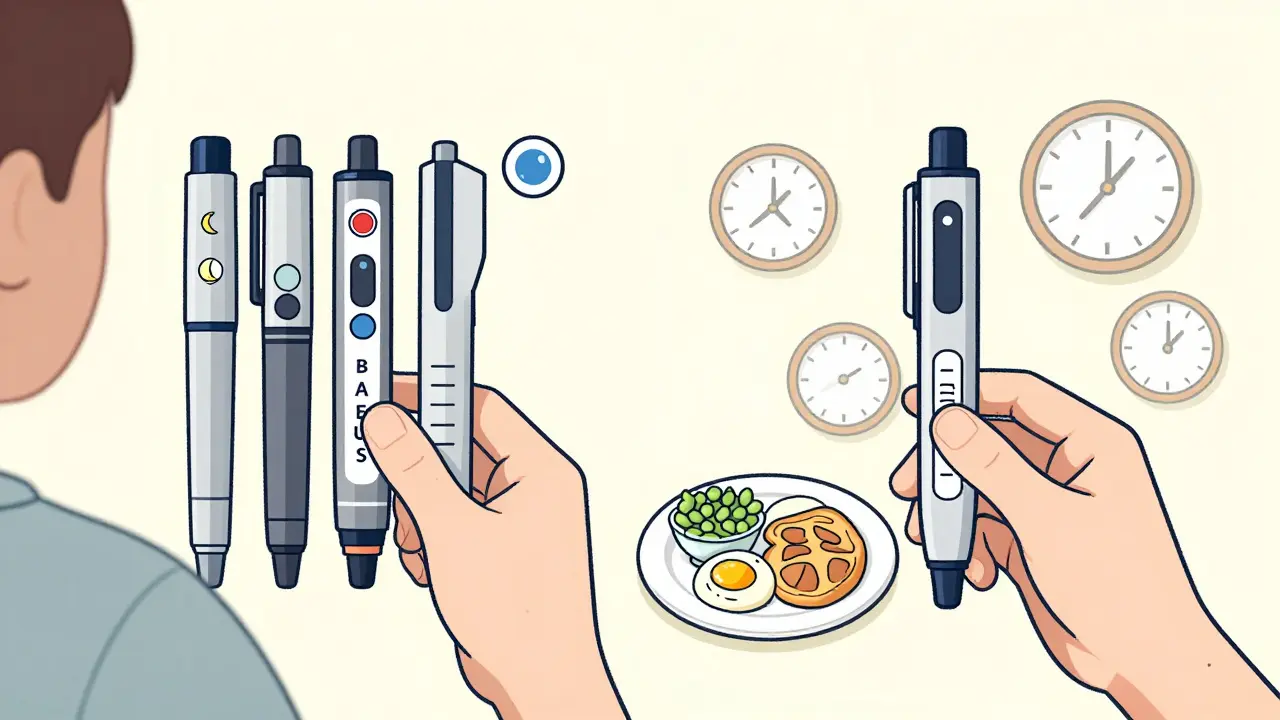
Basal-bolus therapy is like having two separate insulin systems working together. One is a long-acting insulin-think insulin glargine or detemir-that quietly keeps your blood sugar steady between meals and overnight. This is the basal part. The other is a rapid-acting insulin-like insulin glulisine or lispro-taken right before each meal to handle the sugar spike from food. That’s the bolus. You might need four or five injections a day: one or two for basal, and one before each meal. Some people even add a correction dose if their blood sugar is too high.
Premixed insulin is simpler in structure but less flexible. It’s a fixed blend of intermediate-acting insulin (like NPH) and rapid- or short-acting insulin (like regular). Common ratios are 70/30 or 75/25-meaning 70% long-acting, 30% fast-acting. You take it twice a day, usually before breakfast and dinner. It’s one shot that does two jobs: covers your background need and handles mealtime sugar. But because the ratio is fixed, you can’t adjust one without affecting the other.
Side Effects: Hypoglycemia Is the Big One
If you’ve ever felt shaky, sweaty, or confused because your blood sugar dropped too low, you know hypoglycemia isn’t just uncomfortable-it’s dangerous. And this is where the two regimens diverge sharply.
Studies show premixed insulin carries a higher risk. A 2015 trial published in PMC was stopped early because over half the people on premixed human insulin (30/70) had low blood sugar episodes. Why? Because the fixed ratio doesn’t adapt. If you eat less than planned, skip a meal, or exercise after your shot, you’re still getting the full dose of fast-acting insulin. That’s a recipe for a crash.
Basal-bolus users have more control. They can skip a bolus if they don’t eat, or reduce it if they’re eating light. Their basal insulin is steady, not spiked. This flexibility means fewer lows. A 2014 meta-analysis found no statistically significant difference in overall hypoglycemia rates between the two-but that’s because the study grouped all types of lows together. When you look at severe lows or those happening overnight, basal-bolus wins. The risk isn’t zero, but it’s far more manageable.
What About Weight Gain?
Weight gain is common with insulin, no matter the type. But the numbers tell a clear story. People on premixed insulin gained about 1.0 kg on average. Those on basal-bolus gained nearly twice as much-1.9 kg. At first, that seems backward. Shouldn’t more insulin mean more weight gain?
Actually, no. The reason is dosing. Premixed insulin requires higher total daily doses-around 0.72 units per kg of body weight-because it’s less precise. You’re forced to give more long-acting insulin to cover meals, even if you don’t need it. That extra insulin promotes fat storage. Basal-bolus uses less total insulin overall because it’s targeted. You give only what’s needed, when it’s needed. So while both regimens can cause weight gain, basal-bolus tends to be more efficient, not more aggressive.
Lifestyle Fit: Flexibility vs Routine
Here’s where real life hits hard.
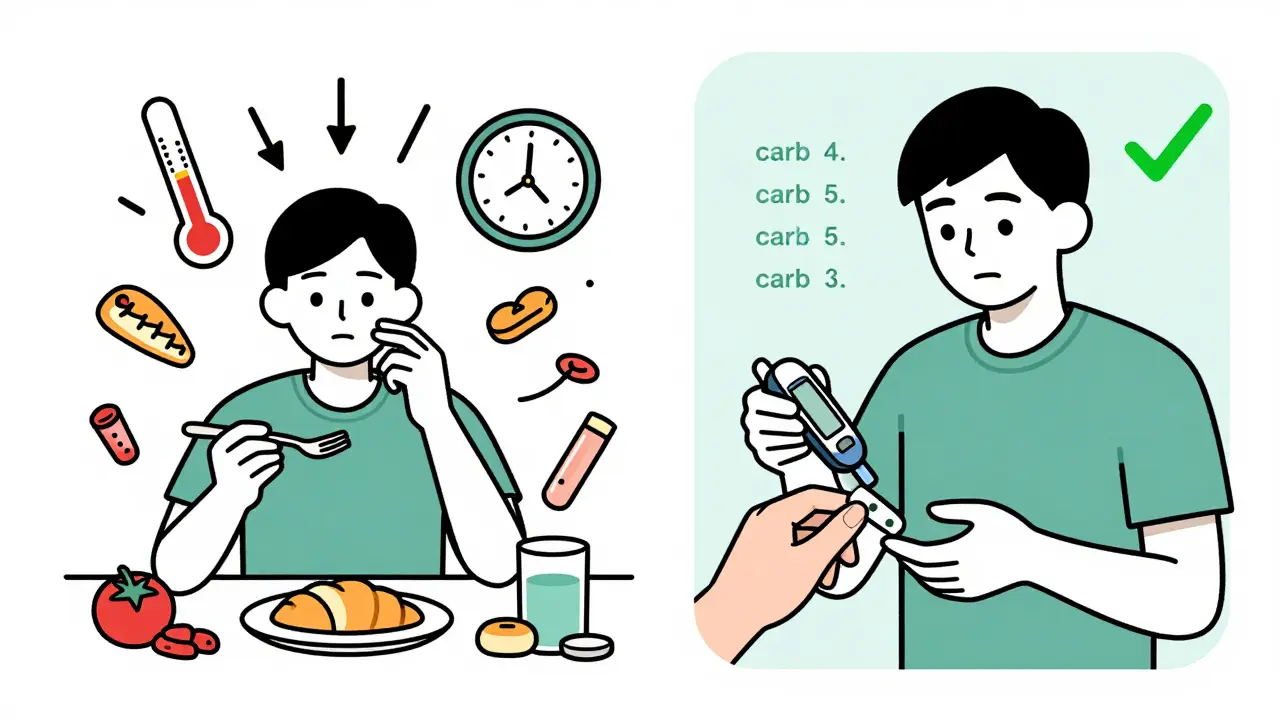
Basal-bolus demands a lot. You need to count carbs. You need to check your blood sugar before every meal. You need to adjust doses based on activity, stress, or illness. It’s not just about injecting-it’s about thinking. For someone with a busy job, irregular shifts, or kids to care for, that’s a heavy lift. But if you’re willing to learn, the payoff is freedom. You can eat dinner at 8 p.m. or skip a snack without fear. You can go out for sushi on Friday and still stay in range.
Premixed insulin is the opposite. It’s rigid. You must eat the same amount of carbs at the same time every day. No skipping meals. No last-minute changes. If you’re a shift worker, a student with erratic class times, or someone who just doesn’t like being tied to a schedule, this can feel like a cage. One Reddit user wrote: “I switched from premixed to basal-bolus because I couldn’t handle the rigid meal schedule-missing a meal meant risking hypoglycemia even if my blood sugar was normal.”
But for others, that rigidity is a relief. An elderly patient on the ADA forum shared: “Two shots a day instead of four has made managing my diabetes possible since my arthritis makes multiple injections painful.” For people with limited dexterity, memory issues, or cognitive decline, fewer injections and less math can mean better adherence and fewer complications.
Real-World Outcomes: HbA1c and Satisfaction
Does one work better? The data is mixed, but the trend is clear.
Basal-bolus consistently achieves lower HbA1c levels. In one 2014 study, 63.5% of people on basal-bolus hit their target of under 7%, compared to just 50.8% on premixed insulin. Another study showed a 0.33% greater HbA1c drop with glargine-glulisine versus premixed. That might sound small, but in diabetes, every 0.5% drop reduces complication risk by 20%.
But here’s the twist: satisfaction matters just as much. The same 2013 study found people on basal-bolus reported significantly higher quality of life and were 50% more likely to stick with their regimen long-term. They felt more in control. Less like a patient. More like someone managing their health.
On the flip side, premixed insulin users often report lower frustration. Fewer injections. Fewer decisions. That’s why, despite higher hypoglycemia risk and less precise control, it’s still used in 35% of global insulin prescriptions. In Asia, it’s even higher-55%-because of cultural meal patterns and provider habits.

Who Gets Which?
Guidelines from the American Diabetes Association and the American Association of Clinical Endocrinologists are clear: basal-bolus is the gold standard for most people who can handle it. Especially for type 1 diabetes, or type 2 with high post-meal spikes. But it’s not for everyone.
Premixed insulin still has a place. It’s often chosen for:
- Older adults with arthritis or memory issues
- People with limited access to diabetes education
- Those who refuse multiple daily injections
- Patients in low-resource settings where monitoring tools are scarce
Meanwhile, basal-bolus works best for:
- People who eat irregular meals
- Those who are tech-savvy and use CGMs
- People with active lifestyles-athletes, shift workers, travelers
- Anyone who wants tighter control and fewer lows
The New Middle Ground: Basal-Plus and Tech
Things are changing. In 2023, the FDA approved the first “basal-plus” insulin-Tresiba with optional Fiasp for meals. It’s not full basal-bolus, but it’s less rigid than premixed. You get the steady basal, and you can add a quick dose only if you eat. No more guessing.
And then there’s technology. Continuous glucose monitors (CGMs) are cutting the hypoglycemia gap. A 2022 study found that premixed users with CGMs had only 0.2 low events per month-far below the 0.8 seen without CGM. AI-driven dosing systems like Diabeloop are also helping. In trials, they cut decision-making steps by 27%. That means less mental load, even for basal-bolus.
By 2030, experts predict basal-bolus will become the standard in high-income countries-not because it’s perfect, but because tech is making it easier.
Final Thought: It’s Not About What’s Better. It’s About What Fits.
There’s no one-size-fits-all insulin plan. Basal-bolus gives you precision and freedom but asks for effort. Premixed gives you simplicity but demands routine. The best choice isn’t the one with the lowest HbA1c or the fewest side effects. It’s the one you can live with for decades.
If you’re struggling with lows, or your meals are unpredictable, talk to your provider about switching. If you’re overwhelmed by counting carbs or juggling four shots a day, ask about basal-plus or CGM support. You don’t have to choose between control and convenience. The tools are getting better. And so are the options.
Can I switch from premixed insulin to basal-bolus?
Yes, many people do. But it’s not a simple swap. You’ll need to learn carb counting, adjust doses based on blood sugar, and possibly use a CGM. Your healthcare team should guide you through a gradual transition, usually over 4-6 weeks. Don’t try to switch on your own-this requires careful monitoring to avoid dangerous lows or highs.
Why do some people gain more weight on basal-bolus?
They don’t. Actually, people on premixed insulin tend to gain more weight on average. The reason? Premixed regimens require higher total daily insulin doses because they’re less precise. Extra insulin promotes fat storage. Basal-bolus uses less insulin overall by matching doses more closely to actual needs. Weight gain happens with any insulin, but basal-bolus is more efficient.
Is premixed insulin cheaper than basal-bolus?
Yes, usually. In the U.S., Medicare Part D data shows premixed insulins cost about $45.75 per month on average, while basal-bolus regimens cost around $68.20. That’s because basal-bolus requires two or three separate insulin products (basal + multiple bolus types), while premixed is one vial or pen. Cost can be a deciding factor, especially without good insurance.
Can I use a CGM with premixed insulin?
Absolutely-and you should. Continuous glucose monitors help reduce hypoglycemia risk with any insulin regimen. For premixed users, CGMs are especially valuable because they reveal how fixed doses interact with variable meals. Studies show CGM use cuts low-blood-sugar events in half for premixed users. It doesn’t fix the rigidity, but it makes it safer.
Which regimen is better for older adults?
It depends. For older adults with good cognition, steady routines, and no mobility issues, basal-bolus can still work. But for those with arthritis, memory problems, or difficulty with fine motor skills, premixed insulin is often preferred. Fewer injections, less math, and simpler routines reduce the risk of errors. The goal isn’t perfection-it’s safety and sustainability.






February 19, 2026 AT 16:00
Been on basal-bolus for 8 years now. The freedom to eat when I want, skip a meal without panic, or go out for sushi at midnight? Worth every extra injection. I used to hate counting carbs, but now I just eyeball it. My CGM does 90% of the work anyway. No more 3 a.m. lows. No more guilt over skipped snacks. It’s not perfect, but it’s mine.
Also, premixed users: I get it. Two shots a day sounds nice. But if you’re skipping meals or eating irregularly, you’re setting yourself up for a crash. I’ve seen friends go hypoglycemic because they ‘just didn’t feel like eating’ after their premixed shot. It’s not laziness-it’s a system that doesn’t adapt.
And yeah, weight gain is real, but I gained less on basal-bolus. Total daily insulin? Lower. Precision? Higher. You’re not flooding your system with extra long-acting just to cover meals you didn’t eat. That’s the key.
Also, the 70/30 premixed? It’s basically a time bomb if you’re active. I used to hike on weekends. Now I just adjust my bolus. No drama.
TL;DR: If you can handle the learning curve, basal-bolus gives you your life back. Premixed gives you a schedule. Choose your prison.