Every year, over 1.5 million people in the U.S. suffer harm from medication errors. Many of these mistakes happen not because of bad doctors or faulty prescriptions, but because no one has a clear, complete list of what the patient is actually taking. This isn’t just a hospital problem-it happens in clinics, emergency rooms, pharmacies, and even at home when someone sees a new specialist. The fix? A simple, accurate, up-to-date medication list that includes everything: prescriptions, over-the-counter pills, vitamins, supplements, creams, inhalers, and herbal teas. And it’s not just for older adults. Anyone on more than three medications, or those switching doctors or hospitals, needs this.
What Goes on a Complete Medication List?
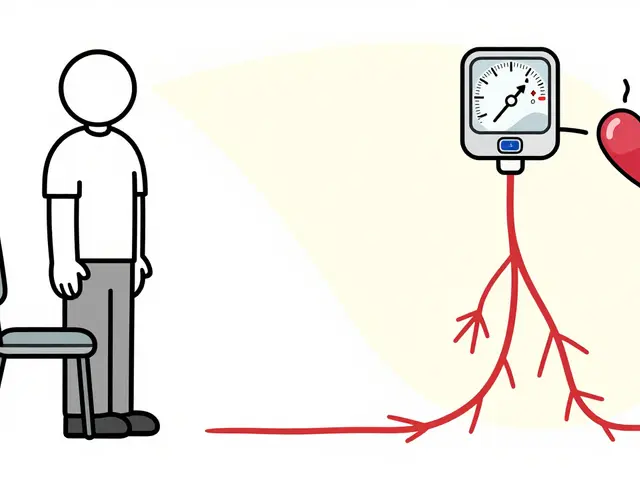
A basic list that just says "blood pressure medicine" won’t cut it. You need details. The FDA’s updated "My Medicines" template, revised in March 2023, spells out exactly what to include:- Medication name: Both generic and brand (e.g., lisinopril 10 mg, not just "BP pill").
- Dosage and frequency: How much and how often (e.g., "take 1 tablet by mouth once daily with breakfast").
- Reason for use: Why are you taking it? (e.g., "for high blood pressure," "for occasional heartburn").
- When you started: The date you began each medication.
- Who prescribed it: Doctor’s name and clinic.
- Refill status: Is it active? Expired? Out of stock?
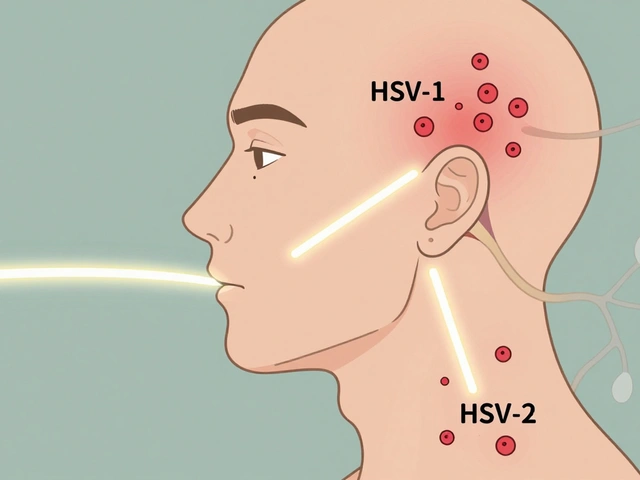
- Allergies and reactions: Not just "penicillin allergy"-specify what happened (e.g., "amoxicillin-rash and swelling").
- Non-oral meds: Eye drops, inhalers, patches, creams, injections.
- Supplements and herbs: Even if you think they’re "natural" or "harmless." St. John’s Wort can interfere with antidepressants. Garlic pills can thin your blood.
- Emergency contact and pharmacy info: Who to call if something goes wrong, and where you fill your prescriptions.
- Last taken time: Especially for as-needed meds like painkillers or anxiety pills. Did you take one yesterday? Today? An hour ago?
Missing any of these? You’re risking a dangerous gap. A 2024 ECRI Institute study found that lists with all these details cut reconciliation errors by 78%. That’s not a small improvement-it’s life-saving.
Why Paper Lists Still Matter (Even in 2026)
You might think apps and digital records are the future-and they are. But right now, 68% of patients still use a paper list, according to the National Council on Aging. Why? Because paper works when the power’s out, when you’re in the ER, or when you’re sitting across from a doctor who doesn’t have your EHR open yet.Handwritten lists should be printed in 12-point font or larger. No cursive. No tiny scribbles. Use a notebook or a printable template from the FDA’s website. Keep it in your wallet, purse, or phone case. Make sure someone else-your spouse, adult child, caregiver-knows where it is.
But don’t stop there. Digital tools are catching up fast. GoodRx, Medisafe, and MyTherapy now have over 150 million combined users, and 42% of GoodRx users actively maintain their medication lists. These apps can send reminders, track refills, and even sync with your pharmacy. The catch? Only 42% of U.S. hospitals connect their electronic records to patient portals where you can update your list. So even if your doctor uses an EHR, you still need your own copy.
The Real Danger: Forgetting the Little Things
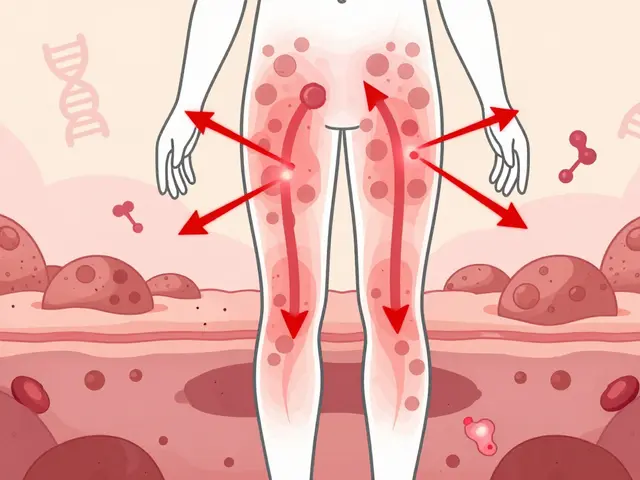
Most people remember their prescriptions. But what about the aspirin you take for headaches? The calcium supplement your sister gave you? The turmeric capsule you started after watching a YouTube video?A 2022 study in the Journal of General Internal Medicine found that 58% of patients forget to mention over-the-counter meds when asked. That’s half of all patients. And it’s not because they’re careless-it’s because they don’t think it matters. But here’s the truth: acetaminophen (Tylenol) can damage your liver if you’re already on other liver-metabolized drugs. Ibuprofen can raise blood pressure and interfere with heart medications. Even vitamin K can cancel out blood thinners like warfarin.
As-needed medications are another blind spot. "Take one for pain" sounds simple. But if you took two last night, one this morning, and another at noon, you might be overdoing it. The ECRI Institute recommends a simple "PRN Tracker"-a small table where you check off each time you take a rescue med. Include the time and reason. It’s not fancy, but it’s accurate.

How to Keep Your List Updated (Without It Becoming a Chore)
A list that’s outdated is worse than no list at all. It gives false confidence. The key is making updates part of your routine.Here’s a simple system:
- Update immediately: Every time you start, stop, or change a dose-do it right away. Don’t wait for your next appointment.
- Set a monthly reminder: Pick one day each month (e.g., the 1st) to review your list. Ask yourself: "Did I get any new meds? Did any get canceled? Did I stop something?"
- Sync your refills: Ask your doctor about 90-day supplies for chronic meds. The AMA found this reduces administrative stress for providers by 65% and improves adherence by 22%.
- Bring it to every visit: Even if your doctor says "we have it in the system," bring your list. Studies show that 68% of medication discussions get cut short during busy appointments. Don’t let yours be one of them.
Patients who follow this routine reduce medication-related hospital visits by 31%, according to the National Council on Aging. That’s not just a number-it’s avoided pain, avoided stress, avoided cost.
What Your Doctor Should Do (And What They Might Not)
Your doctor isn’t just a recipient of your list-they’re part of the process. The American Medical Association’s STEPS Forward program says medication reconciliation should be a standard part of every transition: admission to hospital, discharge, referral to specialist, or even a change in pharmacy.But here’s the problem: 40-60% of medication histories taken by providers contain errors, especially when relying on patient memory alone. A 2024 study by the Institute for Safe Medication Practices found that 73% of patient-reported lists had at least one major omission or mistake.
That’s why doctors should cross-check your list with your pharmacy records. Ask them: "Can you verify this list against my pharmacy’s system?" Most hospitals now have electronic reconciliation tools-87% according to HIMSS. But only 42% let patients update their own lists in the portal. Push for access. You have a right to it under the 21st Century Cures Act, which requires EHRs to give patients real-time access to their meds.

Special Cases: Complex Regimens and Elderly Patients
If you’re taking five or more medications, you’re in a high-risk group. Color-coding helps. Use a highlighter: red for blood thinners, blue for heart meds, green for painkillers. Add icons: a clock for daily meds, a star for as-needed. A 2023 study by Advanced Psychiatry Associates showed this improved adherence by 27%.For older adults, digital tools can be overwhelming. Only 28% of people over 75 can use medication apps without help. That’s why paper lists, with large print and clear labels, remain essential. If you’re helping an aging parent, sit down with them monthly. Don’t assume they remember everything. Check their pill bottles. Look in their medicine cabinet. Ask about supplements they got from friends or online.
The Bigger Picture: Why This Isn’t Just About You
Medication safety isn’t a personal responsibility-it’s a system-wide issue. As of January 2024, Medicare penalizes hospitals that score below 85% on medication reconciliation accuracy. That means your list doesn’t just protect you-it helps your hospital avoid fines.And it’s not just about hospitals. The FDA has invested $4.7 million through 2025 to standardize medication lists. The HL7 FHIR Medication Knowledge Guide, updated in March 2024, is creating a universal format so your list can move safely between clinics, pharmacies, and apps. By 2027, every patient in the U.S. will have access to a consolidated, real-time medication record.
But until then? You’re the most important link in the chain. No app, no EHR, no nurse can replace the accuracy of a patient who knows exactly what they’re taking-and why.
Start Today: Your 10-Minute Action Plan
You don’t need to wait for your next appointment. Do this now:- Grab all your pill bottles, boxes, and supplement containers.
- Write down every item using the FDA’s full list of required details.
- Call your pharmacy and ask for a printout of your current prescriptions.
- Compare the two. Add anything missing.
- Make two copies-one for your wallet, one for a family member.
- Set a calendar reminder: "Medication Review-First of Every Month."
That’s it. Ten minutes. No apps needed. No fancy tech. Just clarity. And that clarity? It’s the difference between a safe care transition and a preventable error.
Do I need to include vitamins and supplements on my medication list?
Yes. Vitamins, herbal remedies, and supplements can interact with prescription drugs. For example, St. John’s Wort can reduce the effectiveness of birth control pills and antidepressants. Garlic or ginkgo biloba can increase bleeding risk if you’re on blood thinners. Even common ones like calcium or vitamin D can interfere with thyroid or kidney medications. Always include them.
What if I forget to take a medication? Should I still list it?
Yes. Your list should reflect what you were prescribed, not what you remembered to take. If you stopped a medication, write "discontinued" and the date. If you’re skipping doses, tell your doctor. Your list is meant to show your full treatment plan-not your adherence record. But if you’re consistently missing doses, that’s something your provider needs to know to adjust your plan.
Can I use my phone’s notes app for my medication list?
You can, but it’s not ideal. Phone notes aren’t always backed up, and they’re not accessible if your phone dies or you’re in an emergency. Use a dedicated app like GoodRx or MyTherapy, or keep a printed copy. If you use your phone, make sure someone else knows how to access it, and turn on auto-backup.
How often should I update my medication list?
Immediately after any change-new prescription, stopped med, changed dose. Also, review it once a month. Even if nothing changed, check for expired meds or bottles you no longer use. Many people keep old meds around and forget to remove them from their list. That’s dangerous.
My doctor says they have my list in their system. Why do I still need my own?
Because systems don’t talk to each other perfectly. Your primary care doctor’s EHR might not have your specialist’s notes. The ER won’t have access to your clinic’s records during an emergency. Even within the same hospital, different departments sometimes use different systems. Your personal list is the only version that’s always with you-and always accurate.
Is it safe to carry my medication list in my wallet?
Yes, and it’s recommended. Keep a printed copy in your wallet, purse, or phone case. If you’re in an accident or collapse, first responders will look for medical info in your wallet. Make sure it’s legible, up-to-date, and includes emergency contacts. Avoid laminating it-some EMS teams need to write on it during emergencies.
Can a medication list help me avoid drug interactions?
Absolutely. A complete list lets your doctor or pharmacist spot dangerous combinations before you take them. For example, mixing certain painkillers with blood pressure meds can cause kidney damage. Taking multiple sedatives together can slow your breathing. A full list makes these risks visible so they can be avoided.
What if I don’t know the generic name of my medication?
Look at the bottle. The generic name is always listed. If you can’t read it, call your pharmacy. They can tell you the generic name and confirm the dosage. You can also search the brand name on Drugs.com or the FDA’s website. Don’t guess. Using only brand names can cause confusion-especially if you switch pharmacies or insurers.


January 26, 2026 AT 07:28
Just printed mine out. Put it in my wallet. Took 8 minutes. Life’s too short to guess what’s in my body.