Biosimilars: What They Are, How They Work, and Why They Matter
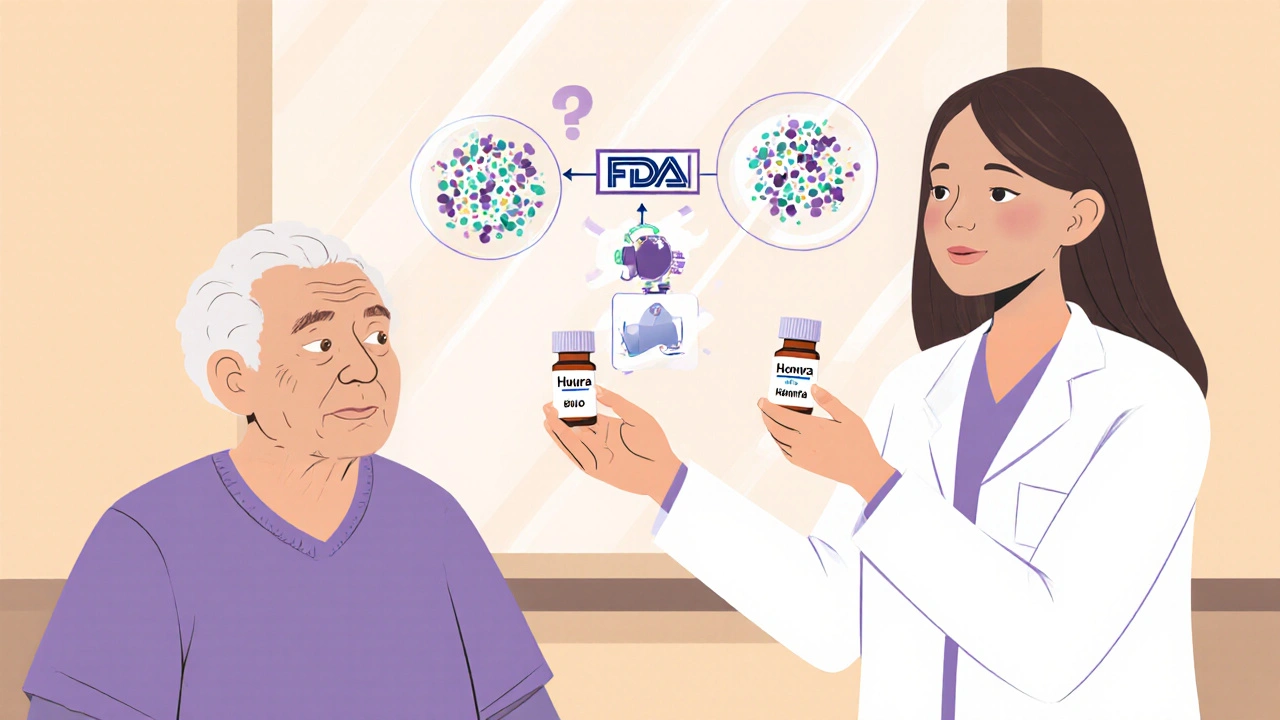
When you hear biosimilars, highly similar versions of complex biologic drugs that are approved after the original patent expires. Also known as biologic generics, they are not exact copies like traditional pills, but they work the same way in the body and are held to strict safety standards. Unlike regular generics, which are made from chemicals, biosimilars come from living cells—think proteins, antibodies, or enzymes—and that makes them much harder to replicate exactly. Still, they must prove they match the original drug in safety, purity, and strength before the FDA or other regulators approve them.
Why does this matter? Because biologic drugs, targeted treatments for cancer, autoimmune diseases, and chronic conditions like rheumatoid arthritis or Crohn’s disease can cost over $100,000 a year. Biosimilars cut those prices by 15% to 35%, sometimes more, making treatments accessible to more people. They’re not cheaper because they’re weaker—they’re cheaper because competition finally entered the market. The same bioequivalence, the scientific process used to prove a biosimilar behaves the same as the original drug in the body that’s used for regular generics is applied here, but with far more complex testing. Studies show patients switching from the original biologic to a biosimilar don’t see a drop in effectiveness or safety.
Some people worry biosimilars are risky, but the data doesn’t back that up. The FDA has approved over 30 biosimilars since 2015, and millions of patients have used them. They’re used for the same conditions as their reference drugs: diabetes, multiple sclerosis, psoriasis, and more. You won’t find biosimilars for every biologic yet—many are still under patent—but the list is growing fast. And when they do become available, they’re often the first option doctors recommend, not just a last resort.
What you’ll find in the posts below are real-world examples of how biosimilars fit into everyday care. You’ll see how they compare to the original drugs, how pharmacists handle prescriptions, what patients need to know before switching, and why some doctors still hesitate to prescribe them. You’ll also find deep dives into related topics like pharmacokinetic testing and partial AUC—tools used to prove biosimilars work just like the originals. This isn’t theory. It’s practice. And it’s changing how medicine is paid for, prescribed, and taken.
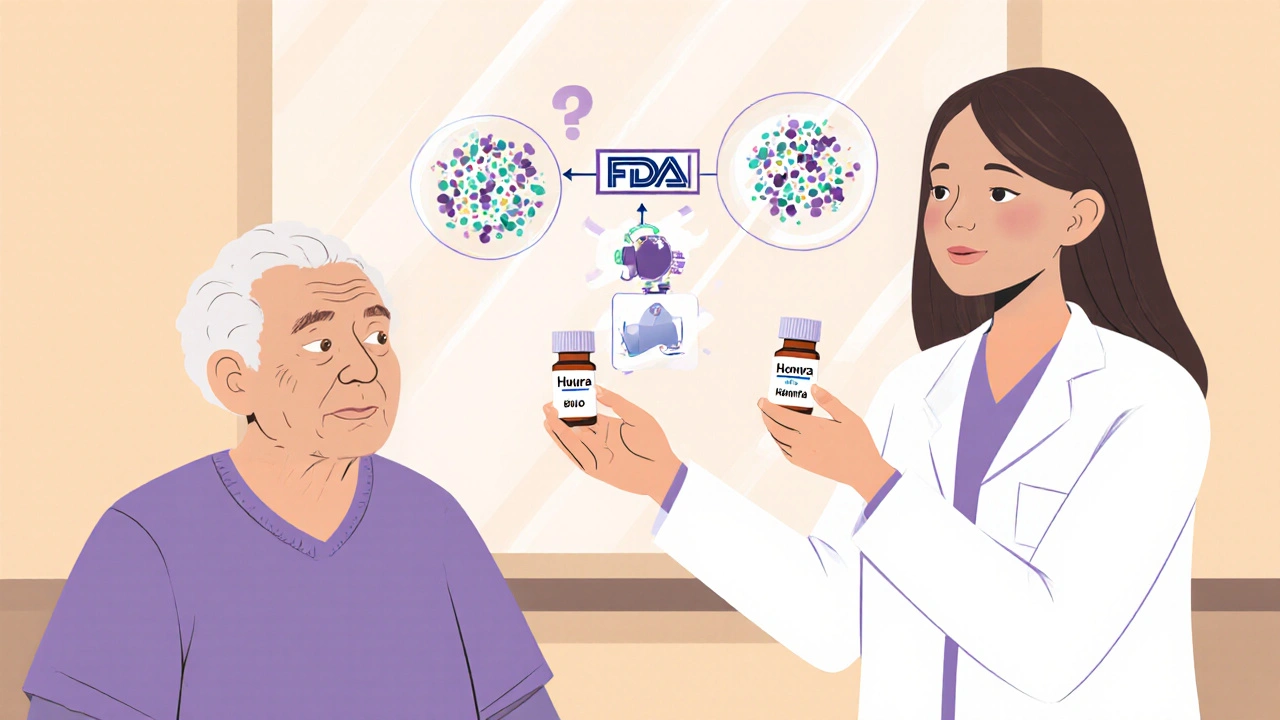
Pharmacists play a vital role in biosimilar adoption by counseling patients, ensuring safe substitution, and overcoming prescriber resistance. Unlike generics, biosimilars require specialized knowledge and careful communication to build trust and improve access to affordable biologic treatments.