CDAI: Understanding the Crohn's Disease Activity Index for Better Management
When you're living with Crohn's disease, a chronic inflammatory condition that affects the digestive tract. Also known as inflammatory bowel disease, it doesn't just cause discomfort—it can change how you live, work, and eat. The CDAI, the Crohn's Disease Activity Index, a standardized tool used by doctors to measure how active the disease is is one of the most common ways to track whether your treatment is working. It’s not a blood test or scan—it’s a simple, calculated score based on how you feel.
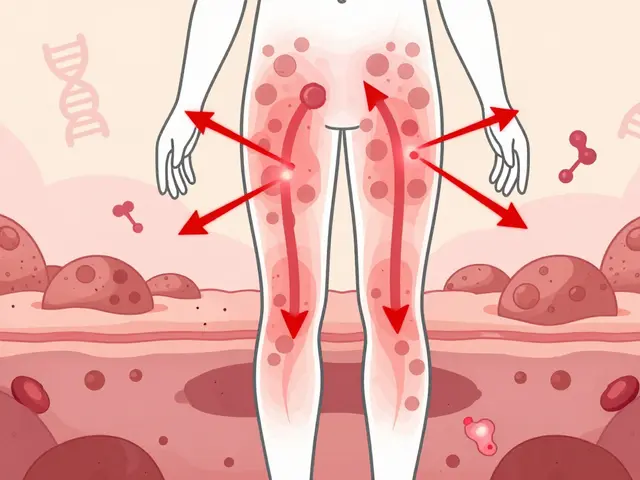
The CDAI looks at eight key factors: number of liquid stools, abdominal pain, general well-being, complications like abscesses or fistulas, use of anti-diarrheal meds, body weight, hematocrit levels, and whether you have a palpable abdominal mass. Each of these adds up to a single number. A score under 150 usually means your disease is in remission. Between 150 and 450? That’s moderate activity. Above 450? That’s severe. It’s not perfect—some people feel worse than their score suggests, and others feel fine even with high scores—but it’s the best tool doctors have for making consistent decisions over time. It’s also used in clinical trials to test new drugs, which means your CDAI score might influence whether a new treatment becomes available to you.
What makes CDAI different from other measures is that it’s patient-centered. It doesn’t rely only on lab results or imaging—it asks you how you’re doing. That’s why it’s so useful in real life. If your score jumps after a vacation or during stress, your doctor can adjust your meds before things get worse. If your score stays low even when you feel tired, it might mean you need to look at sleep, nutrition, or mental health—not just your gut. And because it’s been used for decades, there’s a huge amount of data behind it. You’re not just tracking your own symptoms—you’re part of a larger understanding of how Crohn’s behaves.
There are newer tools out there, like the Harvey-Bradshaw Index, which is simpler but less detailed, or fecal calprotectin tests that measure gut inflammation directly. But CDAI still holds ground because it captures the full picture: how you feel, what’s happening inside, and how your body responds. It’s the bridge between your daily experience and your medical plan.
In the posts below, you’ll find real-world advice on how CDAI scores connect to treatment choices, what to do when your score doesn’t match how you feel, how to track symptoms at home, and how to talk to your doctor using this tool. You’ll also see how CDAI fits into broader care for Crohn’s—like diet, stress, and medication changes. Whether you’re newly diagnosed or have been managing this for years, these guides give you the practical knowledge to use CDAI as a tool for control, not confusion.

CDAI, DAS28, and imaging are key tools for tracking rheumatoid arthritis. Learn how each works, when to use them, and why combining them leads to better outcomes and less joint damage.