Chronic Obstructive Pulmonary Disease (COPD): What to Know
COPD is a long-term lung condition that makes breathing harder over time. It’s a leading cause of death globally, but many people delay getting help because they think breathlessness is just aging. If you’re getting short of breath doing things you used to do easily, this page will give clear, practical steps to find answers and feel better.
How COPD shows up
Common signs include a cough that won’t go away, regular mucus production, wheezing, and feeling short of breath during activity. Symptoms often start slowly. You might notice you avoid stairs or stop walking as fast. Pay attention when colds last longer than before or you need more inhaler use than usual.
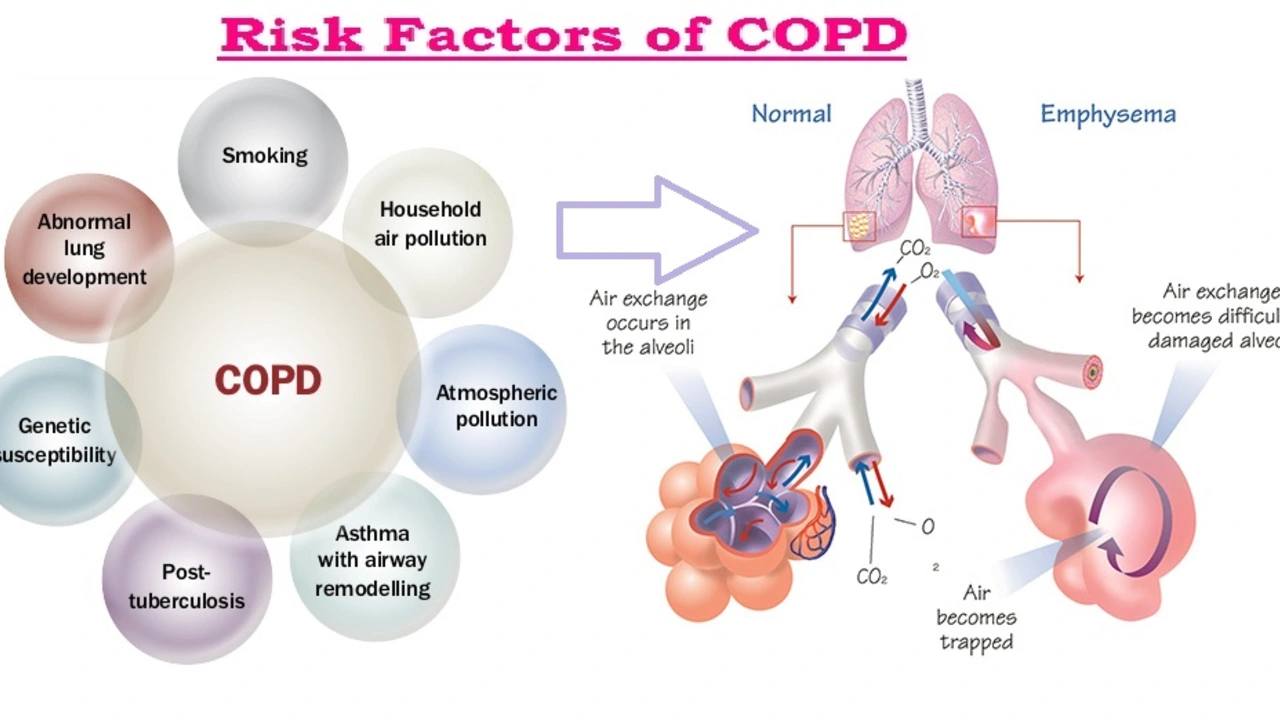
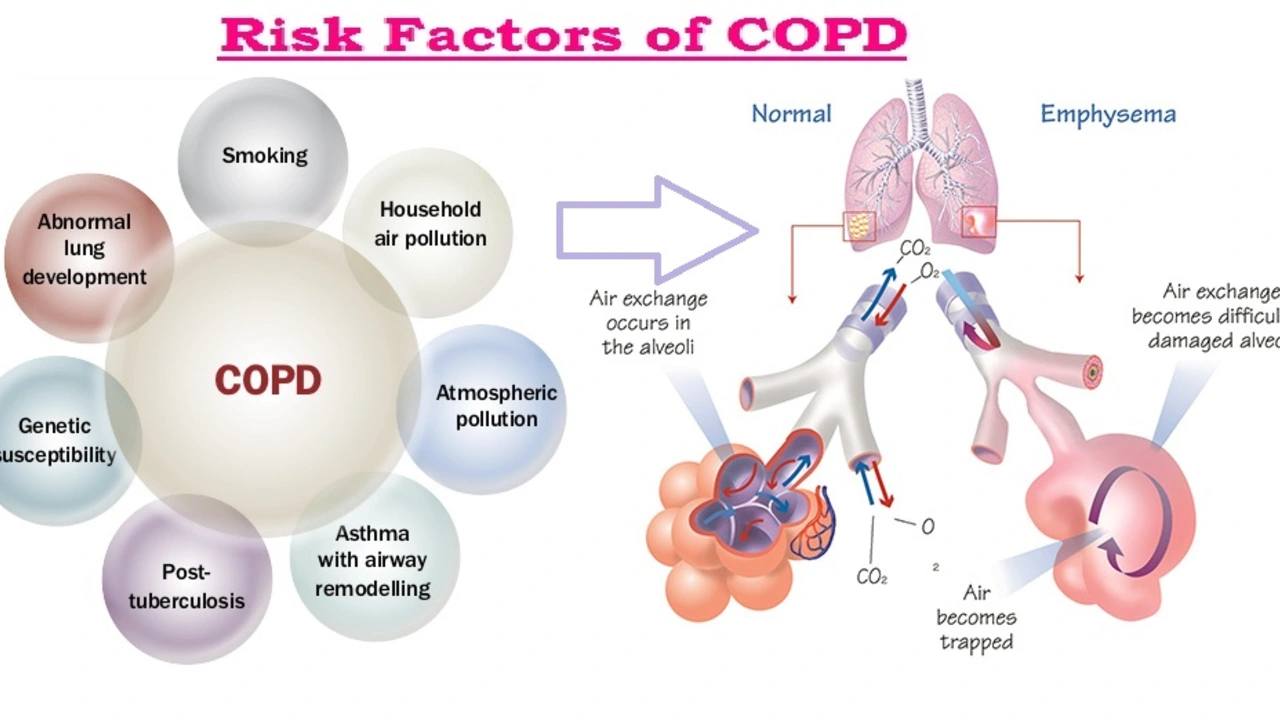
Two main problems cause COPD symptoms: chronic bronchitis (inflamed airways making mucus) and emphysema (air sacs losing elasticity). Most people have a mix of both. Smoking is the main cause, but long-term exposure to air pollution, workplace dust, or a rare genetic issue called alpha-1 antitrypsin deficiency can also lead to COPD.
Getting a diagnosis and tests
Start with your doctor. They’ll ask about symptoms, smoking history, and exposures. The key test is spirometry — a simple breathing test that measures how much air you can blow out and how fast. Chest X-rays or CT scans can show lung damage. Blood tests and oxygen checks help decide how severe your condition is and guide treatment.
Treatment aims to slow damage, ease symptoms, and prevent flare-ups. If you smoke, quitting is the single most effective step. Medicines commonly used include bronchodilators (open airways) and inhaled steroids (reduce inflammation) — often in combination. Short courses of oral steroids or antibiotics may be needed for flare-ups.
Other treatments include pulmonary rehabilitation (supervised exercise, breathing techniques, and education), oxygen therapy for low blood oxygen, and vaccinations to prevent flu and pneumonia. In advanced cases, surgery or lung volume reduction procedures are options for selected patients.
Daily life tips: pace yourself, plan rest breaks, use a rescue inhaler as prescribed, and avoid smoke or dusty places. Learn breathing techniques like pursed-lip breathing to reduce breathlessness during activity. Keep a written action plan with your doctor so you know when to call for help.
Watch for warning signs of an exacerbation: increased shortness of breath, more mucus, a change in mucus color, or high fever. Don’t wait — early treatment often prevents hospital stays. Regular check-ups, vaccinations, and staying active through rehab programs all reduce flare-ups and improve quality of life.
If you need help quitting smoking, ask your doctor about counseling and medicines. Small changes add up: better air quality at home, a healthy diet, and controlled weight can make daily breathing easier. You don’t have to accept decline as normal — with the right plan, many people with COPD live active, meaningful lives.
Hello there. Today, we'll be discussing the use of Lincomycin in managing Chronic Obstructive Pulmonary Disease (COPD). It's a fascinating subject as this antibiotic brings new perspectives in managing this lung condition. We'll cover how this medication works, what the recent studies are saying, and how it could be a game-changer in COPD management. This is critical information for COPD patients and healthcare providers alike. I hope you find this useful and insightful!