Ear Infection: Causes, Treatments, and What Really Works
When your ear hurts, it’s not just discomfort—it’s a signal your body is fighting something. An ear infection, an inflammation of the ear, often caused by bacteria or viruses that spread from the nose or throat. Also known as otitis, it can strike the outer ear, middle ear, or inner ear, each with different causes and treatments. Most ear infections in adults and kids start after a cold or allergy flare-up. The Eustachian tube, which connects the middle ear to the back of the throat, gets blocked. Fluid builds up. Bacteria or viruses grow. That’s when the pain, pressure, and sometimes hearing loss kick in.
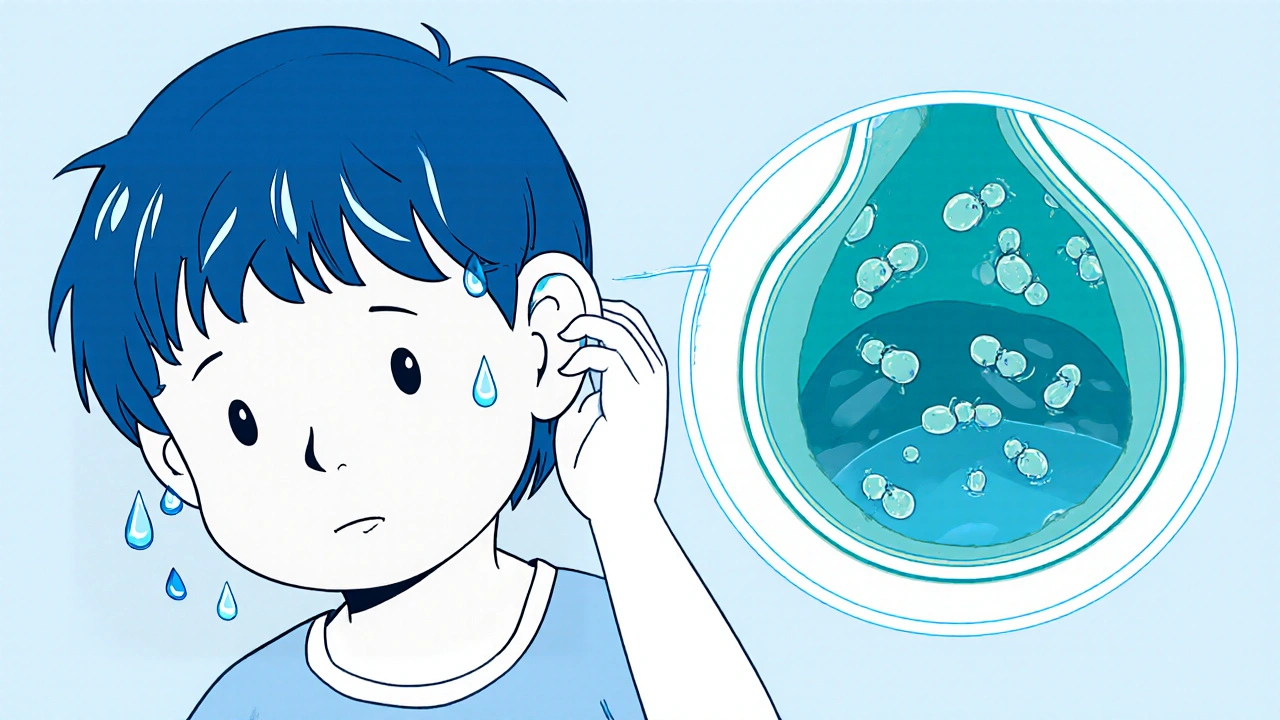
Not all ear infections need antibiotics. In fact, the middle ear infection, the most common type in children, often clears on its own within a few days. Studies show that up to 80% of kids with ear infections get better without pills. But if the pain is severe, fever lasts more than 48 hours, or fluid drains from the ear, that’s when you need to see a doctor. For outer ear infections—often called swimmer’s ear—the fix is usually different. It’s usually caused by water trapped in the ear canal, leading to bacterial growth. That’s where antibiotic ear drops, directly applied to the ear canal to kill infection without affecting the rest of the body work better than oral pills.
What you do at home matters just as much as what the doctor prescribes. Warm compresses help ease pain. Over-the-counter pain relievers like ibuprofen or acetaminophen reduce swelling and discomfort. Avoid putting cotton swabs, oils, or homemade remedies into the ear—that can push debris deeper or damage the eardrum. If you’ve had recurring ear infections, especially in kids, it might be worth checking for underlying issues like allergies, enlarged adenoids, or even silent reflux. And while many people reach for antibiotics right away, overuse leads to resistant strains. That’s why doctors now wait 48 to 72 hours before prescribing, unless symptoms are severe.
The posts below cover exactly what you need to know: how to tell if it’s just water in the ear or something worse, which pain relief methods actually work, when to skip antibiotics, and how certain medications—like those used for allergies or sleep—can accidentally make ear problems worse. You’ll find real-world advice from people who’ve been there, backed by clinical insights. No hype. No guesswork. Just clear steps to feel better faster.
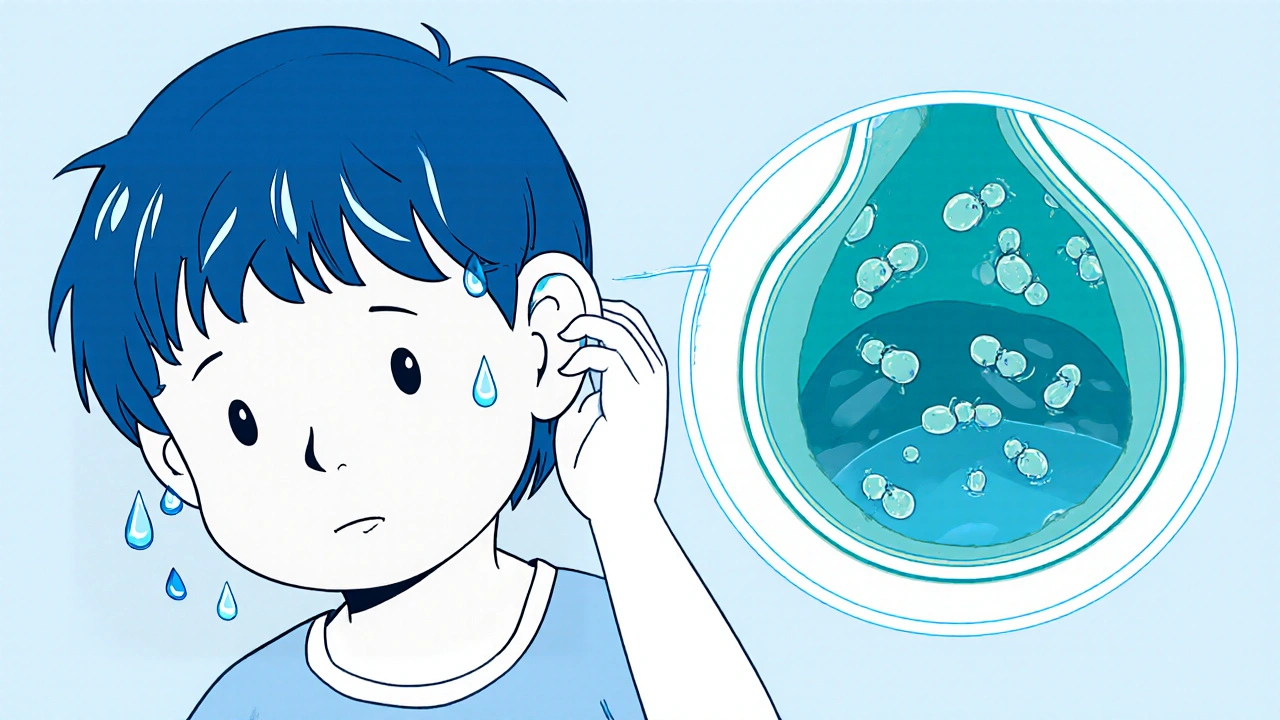
Swimmer’s ear, or otitis externa, is a painful ear infection caused by trapped water and bacterial growth. Learn how to prevent it with simple drying habits and what treatments actually work-backed by clinical data and real patient outcomes.