ERAS Protocol: What It Is and How It Changes Recovery After Surgery
When you hear ERAS protocol, a standardized, evidence-based approach to surgical care designed to speed up recovery and reduce complications. Also known as enhanced recovery after surgery, it’s not just a checklist—it’s a complete rethink of how hospitals handle everything from pre-op fasting to pain control after the cut is closed. This isn’t some experimental trend. Hospitals across the U.S. and Europe have adopted it because patients leave sooner, feel better faster, and have fewer trips back to the ER.
The ERAS protocol, a standardized, evidence-based approach to surgical care designed to speed up recovery and reduce complications. Also known as enhanced recovery after surgery, it’s not just a checklist—it’s a complete rethink of how hospitals handle everything from pre-op fasting to pain control after the cut is closed. This isn’t some experimental trend. Hospitals across the U.S. and Europe have adopted it because patients leave sooner, feel better faster, and have fewer trips back to the ER.
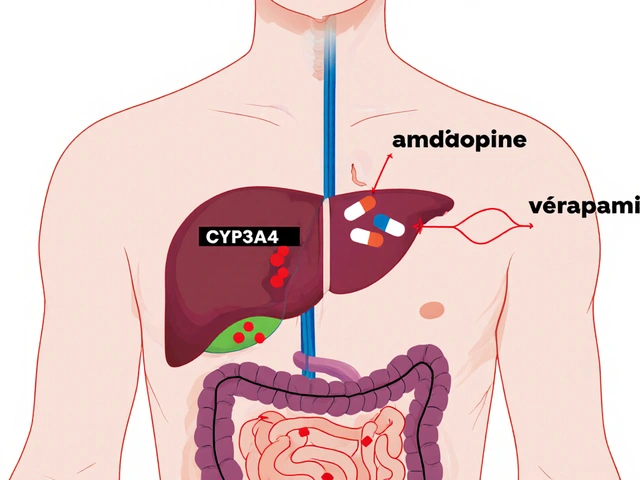
What makes it different? Traditional surgery meant fasting for 12 hours, skipping fluids, using strong opioids, and staying in bed for days. ERAS flips that. You drink carbs before surgery to keep your metabolism stable. You get non-opioid pain meds like acetaminophen and gabapentin instead of relying on morphine. You get up and walk the same day. You eat real food within hours. These aren’t small tweaks—they’re game-changers. And they’re backed by data: studies show patients on ERAS spend up to 30% less time in the hospital and have half the rate of infections and bowel obstructions.
It’s not just about the surgery itself. The ERAS protocol, a standardized, evidence-based approach to surgical care designed to speed up recovery and reduce complications. Also known as enhanced recovery after surgery, it’s not just a checklist—it’s a complete rethink of how hospitals handle everything from pre-op fasting to pain control after the cut is closed. This isn’t some experimental trend. Hospitals across the U.S. and Europe have adopted it because patients leave sooner, feel better faster, and have fewer trips back to the ER.
What makes it different? Traditional surgery meant fasting for 12 hours, skipping fluids, using strong opioids, and staying in bed for days. ERAS flips that. You drink carbs before surgery to keep your metabolism stable. You get non-opioid pain meds like acetaminophen and gabapentin instead of relying on morphine. You get up and walk the same day. You eat real food within hours. These aren’t small tweaks—they’re game-changers. And they’re backed by data: studies show patients on ERAS spend up to 30% less time in the hospital and have half the rate of infections and bowel obstructions.
It’s not just about the surgery itself. The perioperative care, the full cycle of medical attention before, during, and after surgery is redesigned. Nurses, anesthesiologists, surgeons, and even dietitians all follow the same plan. No more conflicting advice. No more "we’ve always done it this way." It’s teamwork built on published guidelines—not guesswork. And it works for everything: colon resections, hip replacements, even heart surgery.
Some patients worry this sounds too good to be true. But the evidence is solid. The postoperative outcomes, the measurable results after surgery, including recovery time, pain levels, and complication rates are better. Fewer readmissions. Less chronic pain. Faster return to work. This isn’t about cutting corners—it’s about doing things smarter. The surgical recovery, the process of healing and regaining function after an operation doesn’t happen by accident. It’s engineered.
Below, you’ll find real-world guides that break down how ERAS works in practice. From how to prepare for surgery without starving yourself, to what pain relief actually works without opioids, to how to avoid the common mistakes that delay healing. These aren’t theory pieces—they’re tools you can use, whether you’re a patient, a caregiver, or a clinician trying to make recovery better.
Postoperative ileus is a common, painful delay in bowel function after surgery-often caused by opioids. Learn how multimodal pain control, early movement, and targeted drugs can prevent it and speed recovery.