IBS Relief: Natural and Medical Ways to Manage Irritable Bowel Syndrome
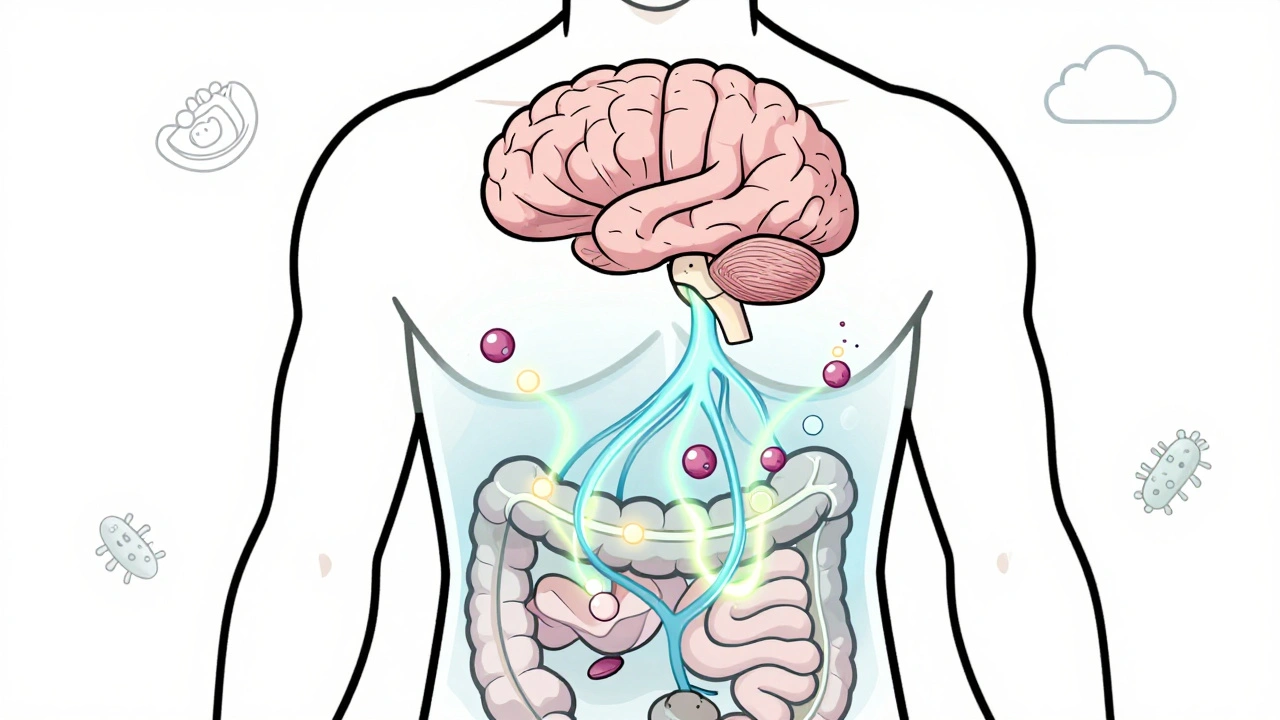
When you live with irritable bowel syndrome, a chronic digestive disorder marked by abdominal pain, bloating, and unpredictable bowel changes. Also known as spastic colon, it doesn’t show up on scans or blood tests—but it can wreck your daily life. Unlike Crohn’s or colitis, IBS isn’t caused by inflammation or damage. It’s a functional problem: your gut talks to your brain, and the signal gets mixed up. Stress, food, and even sleep can trigger flare-ups. The good news? You don’t have to just suffer. Real IBS relief is possible—with the right mix of diet, lifestyle, and targeted treatments.
Many people with IBS find relief by adjusting what they eat. The low-FODMAP diet, a scientifically tested approach that limits fermentable carbs known to trigger gas and bloating has helped millions cut symptoms by up to 70%. Foods like onions, garlic, beans, and certain fruits can be troublemakers. But it’s not about cutting everything forever—it’s about testing, finding your triggers, and rebuilding a safe list. Then there’s gut microbiome, the trillions of bacteria living in your intestines that influence digestion, mood, and immune response. Studies show that probiotics, especially strains like Bifidobacterium infantis, can calm inflammation and reduce bloating. Fiber matters too—but not all fiber is equal. Soluble fiber (like oats and psyllium) often helps, while insoluble fiber (like wheat bran) can make things worse for some.
Medications aren’t a cure, but they can give you back control. Antispasmodics like dicyclomine ease cramping. Laxatives or anti-diarrheals help balance bowel movements. For those with severe symptoms, newer drugs like rifaximin or linaclotide target gut nerves and fluid flow directly. And don’t ignore the brain-gut connection. Cognitive behavioral therapy, a type of talk therapy proven to rewire how the brain responds to gut signals has helped patients reduce pain and anxiety linked to IBS—even when meds failed.
What you’ll find in the posts below isn’t a list of quick fixes. It’s a collection of real, practical strategies backed by research—from how opioids can slow your gut after surgery to how drug interactions might be making your symptoms worse. You’ll see how managing stress, tracking food, and understanding your body’s signals can turn IBS from a daily battle into something you manage—not something that manages you.
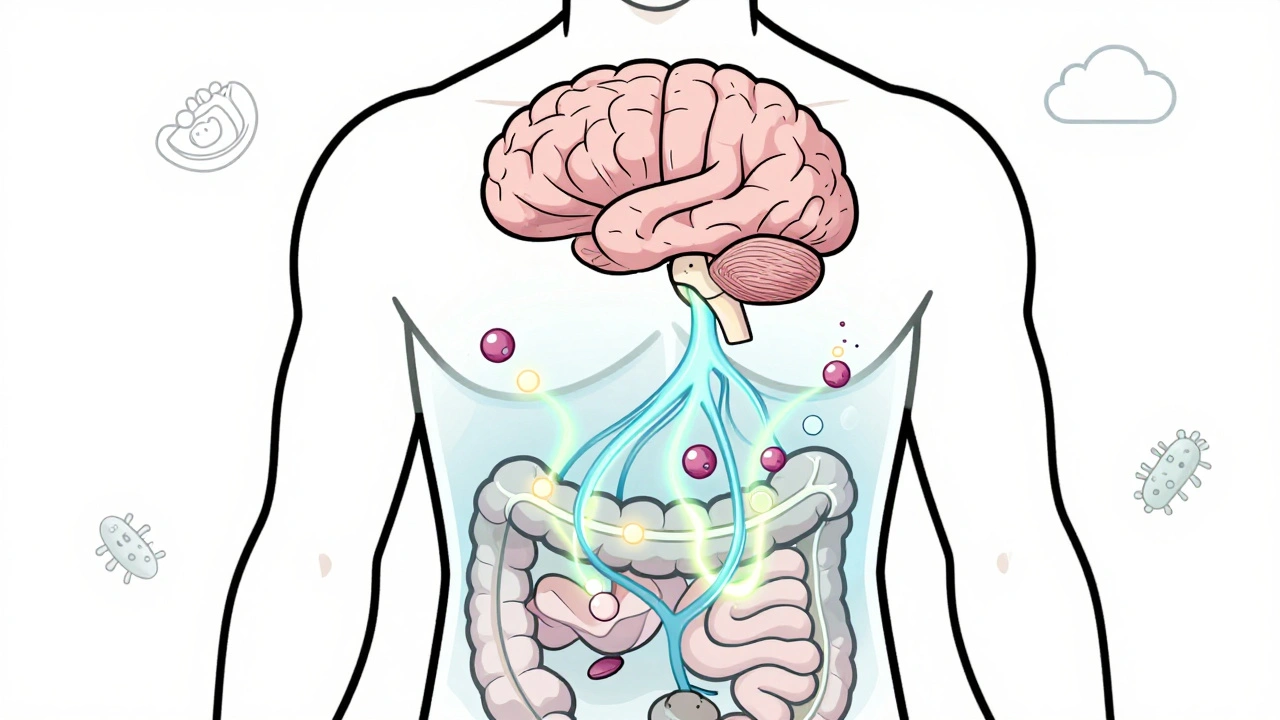
Irritable Bowel Syndrome is not just a digestive issue-it's a breakdown in gut-brain communication. Learn how serotonin, gut bacteria, and brain wiring affect symptoms-and what treatments actually work.