When Not to Use Antibiotics: Know the Risks and Better Alternatives
When you’re sick, it’s easy to assume antibiotics are the answer—but antibiotics, medications designed to kill or slow the growth of bacteria. Also known as antibacterial drugs, they do nothing against viruses like the common cold, flu, or most sore throats. Taking them when they’re not needed doesn’t speed up recovery. It just trains germs to fight back.
Every time you take an antibiotic unnecessarily, you’re helping create antibiotic resistance, a growing global threat where bacteria evolve to survive drug treatment. The CDC calls this one of the biggest public health dangers we face. Superbugs like MRSA and drug-resistant tuberculosis are already killing tens of thousands each year. And it’s not just about you—when you misuse antibiotics, you put your family, neighbors, and future patients at risk.
Most upper respiratory infections are viral. That means antibiotics won’t touch them. A runny nose, cough, or sore throat? Almost always caused by a virus. Even ear infections and sinus infections often clear up on their own without pills. Studies show that over 80% of sinus infections resolve without antibiotics. The same goes for many cases of bronchitis and the common cold. The real problem? Doctors sometimes prescribe them out of habit—or because patients expect them. You don’t need a prescription to feel better. Rest, fluids, and time often do the job.
There are times antibiotics are necessary—like strep throat, pneumonia, or a urinary tract infection. But you can’t tell the difference by symptoms alone. That’s why you need a doctor’s diagnosis. If you’re told you have a virus, don’t push for antibiotics. Ask about safe ways to manage symptoms. For pain and fever, acetaminophen or ibuprofen work better than antibiotics. For congestion, saline sprays and humidifiers help. For coughs, honey (for adults and kids over one) is more effective than many OTC syrups.
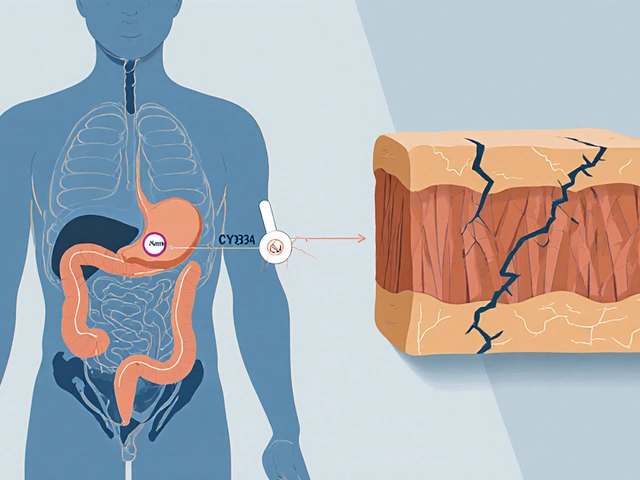
Antibiotics also wreck your gut. They kill good bacteria along with bad, which can lead to diarrhea, yeast infections, and even long-term digestive issues. One course of antibiotics can change your microbiome for months. And if you take them too often, your body stops responding when you really need them.
What you’re about to read isn’t just theory. The posts below cover real cases where antibiotics were misused—and what actually worked instead. You’ll find clear guides on when to skip them, how to spot a true bacterial infection, and what to do when your doctor says yes. You’ll also see how drugs like moxifloxacin, while powerful, carry serious risks if used carelessly. This isn’t about avoiding medicine. It’s about using it right.
Acute bronchitis is usually viral and doesn't need antibiotics. Learn how to manage the cough safely with rest, fluids, honey, and proven remedies-without unnecessary drugs.