Drug Metabolism: How Your Body Processes Medications and What It Means for You
When you take a pill, it doesn’t just sit there waiting to help you. Your body breaks it down—this process is called drug metabolism, the chemical transformation of medications in the body to make them easier to eliminate. Also known as medication biotransformation, it’s what determines how long a drug lasts, how strong it feels, and whether it might cause side effects. This isn’t magic—it’s biology. And it’s different for everyone.
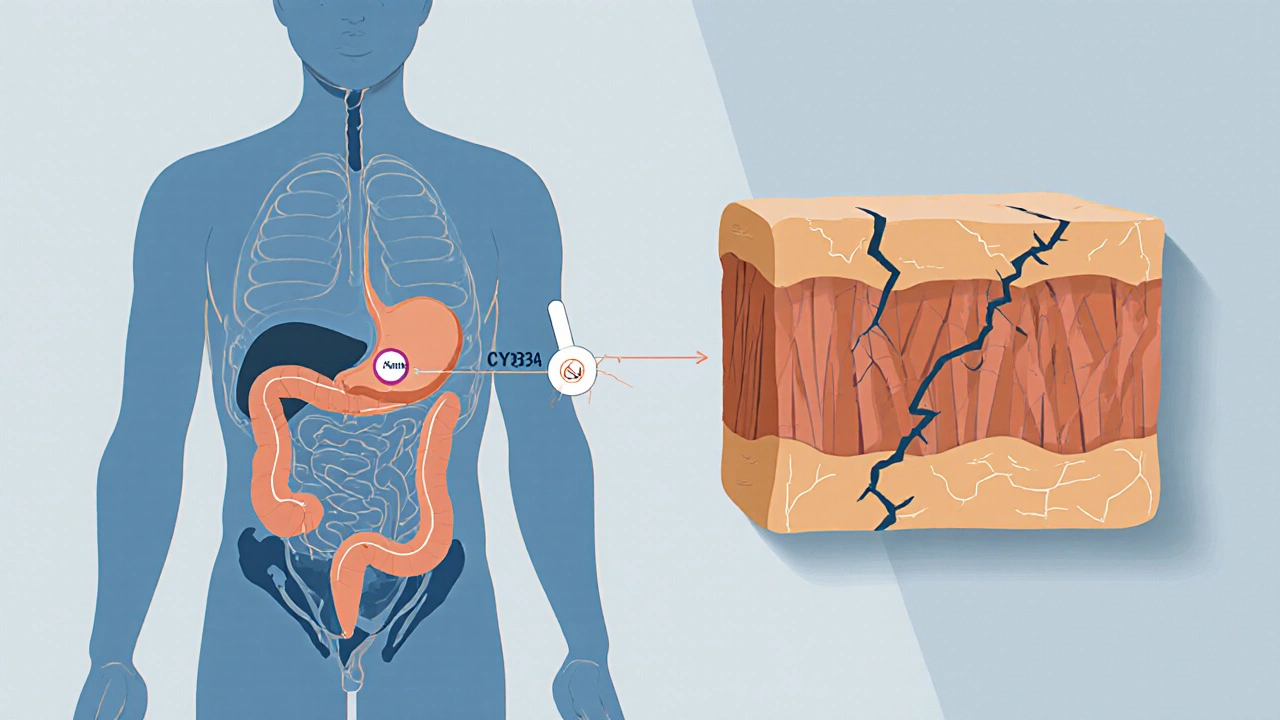
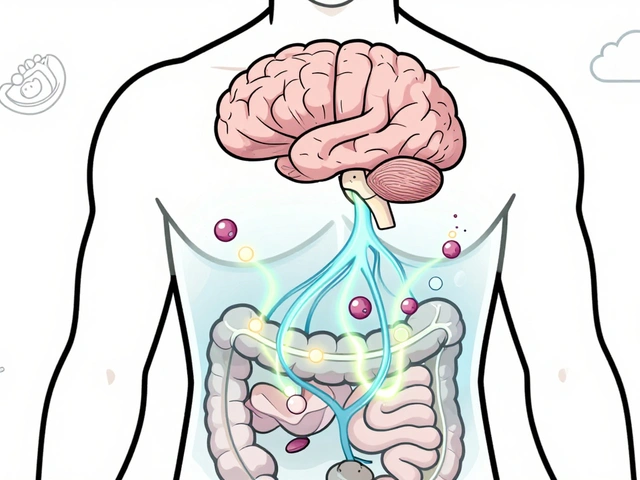
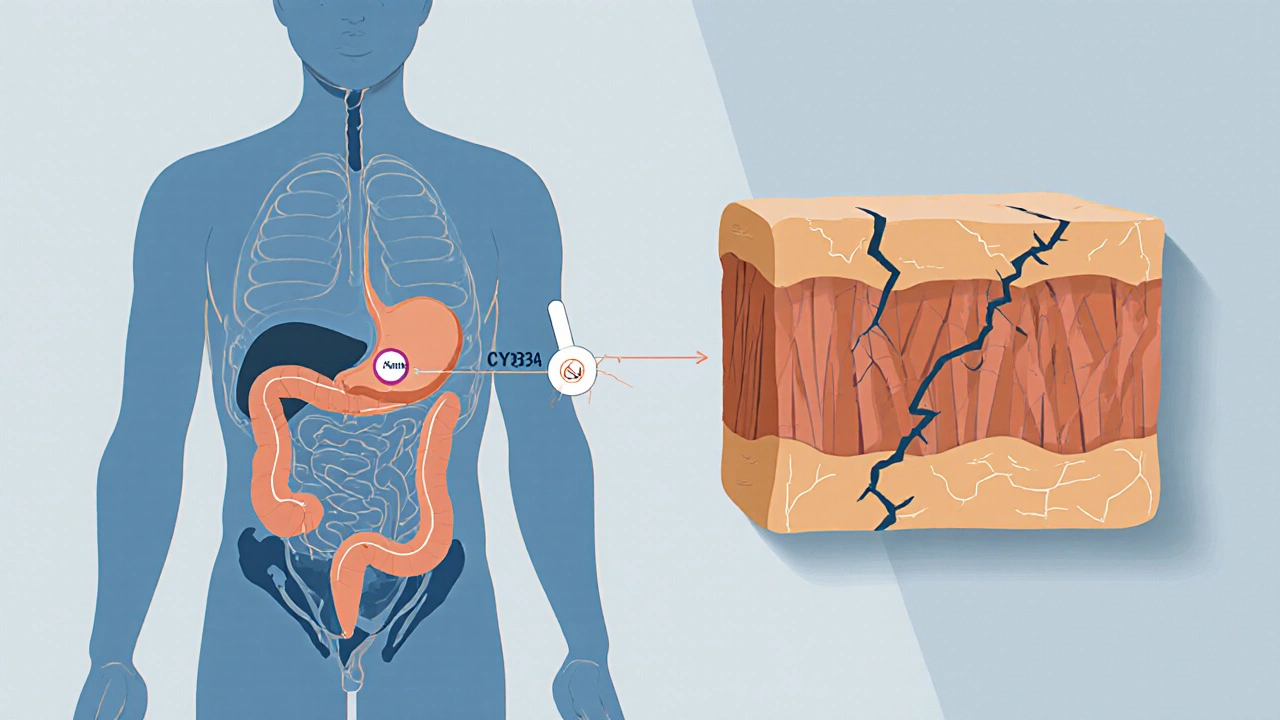
Most of this work happens in the liver enzymes, special proteins, mainly from the CYP450 family, that break down drugs in the liver. These enzymes are like factory workers: some are fast, some are slow, and some get overwhelmed if you take too many drugs at once. That’s why two people taking the same dose of a medication can have totally different experiences. One feels relief; the other feels sick. It’s not about willpower—it’s about your unique enzyme activity. Factors like age, genetics, diet, and other medications all tweak how these enzymes perform. For example, grapefruit juice can shut down key enzymes, causing drugs like statins to build up to dangerous levels. On the flip side, smoking can speed up metabolism, making some drugs less effective.
Then there’s bioavailability, the portion of a drug that actually enters your bloodstream and becomes active. A drug might be perfectly designed, but if your gut doesn’t absorb it well—or your liver destroys it too fast—it won’t help. That’s why some medications come in extended-release forms, or why certain drugs need to be taken with food. It’s all about getting the right amount to the right place at the right time. And when bioavailability drops, so does effectiveness. That’s why switching from brand to generic isn’t always as simple as saving money—it can change how your body handles the drug.
Understanding drug metabolism isn’t just for doctors. If you’ve ever wondered why your antidepressant took weeks to kick in, or why your painkiller stopped working after a few months, the answer lies here. It’s also why some people can’t tolerate statins, why certain ADHD meds trigger heart issues, or why you need to be careful with OTC sleep aids if you’re on other prescriptions. The posts below dig into real cases: how dose adjustments help with statin side effects, why some antihistamines are safer in pregnancy, how creatine affects kidney labs, and what happens when your body metabolizes moxifloxacin differently than expected. These aren’t abstract concepts—they’re daily realities for people managing their health.
What you’ll find here isn’t theory—it’s practical knowledge drawn from real patient experiences and clinical data. Whether you’re trying to reduce side effects, avoid dangerous interactions, or simply understand why your meds behave the way they do, the articles below give you the tools to ask better questions and make smarter choices. No jargon. No fluff. Just what you need to know to stay safe and get results.
Learn the difference between pharmacokinetic and pharmacodynamic drug interactions-how they work, why they matter, and how to avoid dangerous combinations. Real-world examples and expert insights.