Opioid Side Effects: What You Need to Know Before Taking Them
When you take opioids, a class of powerful pain-relieving drugs that include oxycodone, hydrocodone, morphine, and fentanyl. Also known as narcotics, they work by binding to receptors in your brain and spinal cord to block pain signals. But they also affect areas that control breathing, mood, and reward—making them effective for pain but risky for your body. Many people start opioids after surgery or injury, thinking they’re safe because doctors prescribe them. But even short-term use can lead to side effects that aren’t always obvious until it’s too late.
Common opioid side effects, include drowsiness, constipation, nausea, and dizziness. These aren’t just inconveniences—they can stop you from working, driving, or even sleeping normally. Constipation is so widespread that most people on opioids need laxatives just to stay regular. Drowsiness isn’t just feeling tired; it’s a foggy, slow mental state that increases fall risk, especially in older adults. And while nausea might fade after a few days, it’s enough to make people quit their meds early—even when they still need them.
Beyond the obvious, there are deeper risks. opioid dependence, a physical adaptation where your body starts needing the drug to function normally can develop in as little as a week. It’s not addiction—yet—but it means stopping suddenly causes opioid withdrawal, a painful set of symptoms like sweating, diarrhea, muscle aches, and anxiety. Then there’s the real danger: opioid overdose, when breathing slows so much you stop getting oxygen. It can happen if you take too much, mix opioids with alcohol or sleep aids, or if your tolerance drops after a break. Overdose doesn’t always look like a dramatic collapse—it can start with quiet breathing, then silence.
What most people don’t realize is that these side effects aren’t random. They’re predictable. And they’re manageable—if you know what to do. The key isn’t avoiding opioids entirely, but understanding how to use them safely, recognize warning signs, and know when to switch to something else. That’s why the posts below cover everything from non-opioid pain strategies to how to spot early signs of dependence, what to do if you miss a dose, and how to talk to your doctor about reducing your dose without suffering through withdrawal. You’ll find real advice from people who’ve been there, and science-backed ways to protect yourself without giving up pain relief.
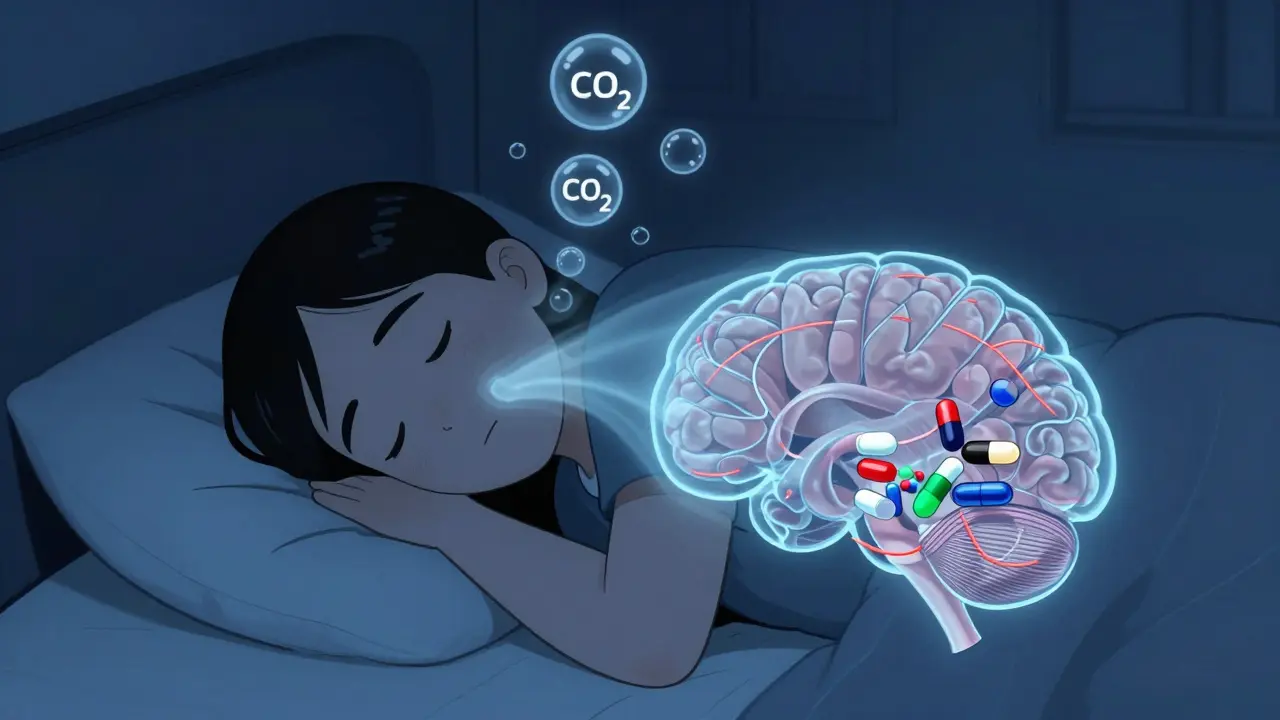
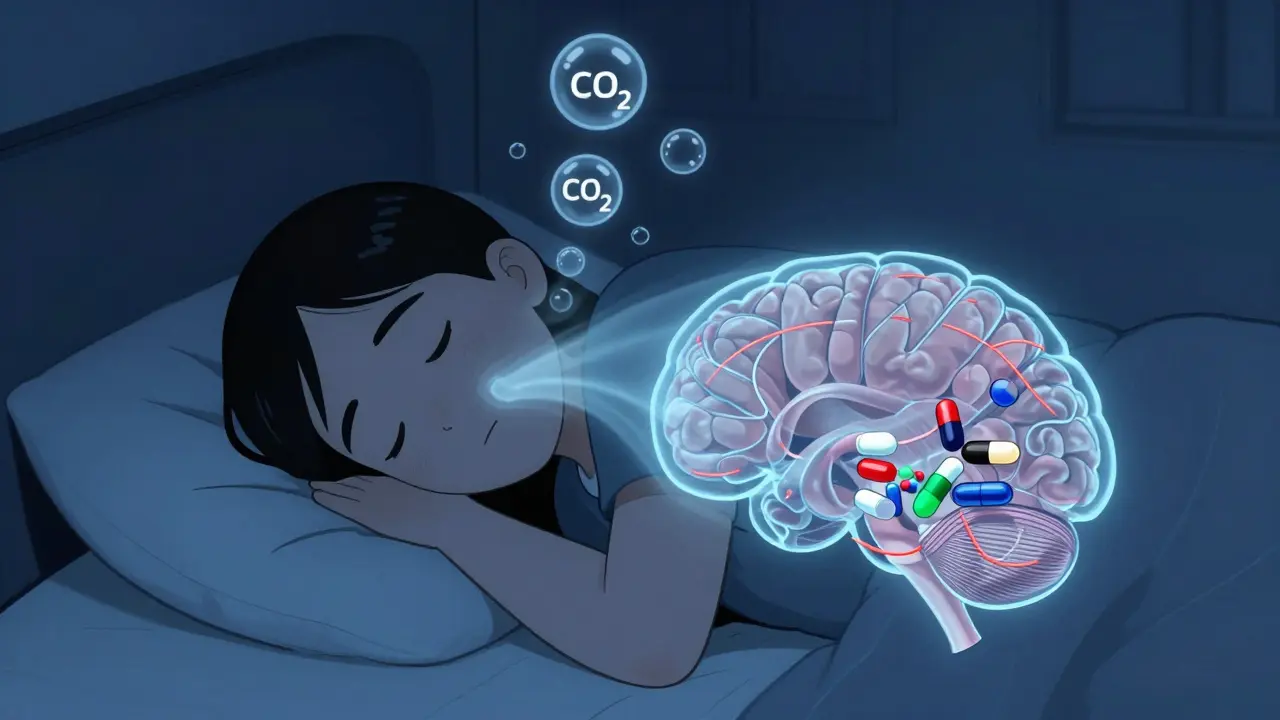
Opioids can cause dangerous breathing pauses during sleep, even in people without prior sleep apnea. This hidden risk leads to overdose deaths at night. Learn how opioids disrupt breathing, who’s most at risk, and what to do to stay safe.
Postoperative ileus is a common, painful delay in bowel function after surgery-often caused by opioids. Learn how multimodal pain control, early movement, and targeted drugs can prevent it and speed recovery.